Terapia Cognitivo-Conductual Psicodélica: sobre la ketamina, el contexto y las competencias en Psicoterapia Asistida
Este trabajo está en proceso. Les pedimos disculpas por cualquier detalle que se nos haya pasado al traducir nuestro contenido humano al español. Traducir esta investigación nos ayuda a que este enfoque terapéutico sea más accesible para más personas. Gracias por tu interés en la psicoterapia asistida con psicodélicos, utilizando ketamina y terapia cognitivo-conductual.
La terapia cognitivo-conductual psicodélica se apoya en más de seis décadas de investigación sobre la ketamina, un medicamento genérico aprobado por la FDA en 1970 y que la OMS incluye en su Lista de Medicamentos Esenciales. En dosis subanestésicas, la ketamina se ha investigado como herramienta psicodélica con aplicaciones en ansiedad, depresión, alcoholismo, manejo del dolor y estrés postraumático.
Contexto clínico y marco regulatorio
En los Estados Unidos y otros países, la psicoterapia asistida por ketamina se desarrolla bajo un marco clínico que considera tanto la seguridad médica como el acompañamiento psicoterapéutico. La telemedicina permite ampliar el acceso, siempre con las debidas precauciones y apoyo profesional.
Competencias del equipo terapéutico
- Profesional médico/psiquiátrico: Evalúa, diagnostica y prescribe, considerando riesgos y beneficios del tratamiento con ketamina.
- Psicoterapeutas y profesionales de la salud mental: Aplican enfoques como la terapia cognitivo-conductual para acompañar la experiencia y favorecer la integración posterior.
- Facilitadores psicodélicos: Pueden brindar apoyo adicional durante la experiencia, aunque no reemplazan a un profesional de salud mental con licencia.
Precauciones y efectos
La ketamina, como otros medicamentos psicodélicos, puede inducir experiencias psicodelicas o visionarias. Estas requieren preparación, apoyo y un marco terapéutico claro. El uso domiciliario supervisado por telemedicina se encuentra en estudio y, cuando está bien indicado, puede ser una opción segura.
Ética profesional
La relación terapéutica nunca incluye conductas sexuales con ningún miembro del equipo de tratamiento psicodélico. Este principio ético protege la seguridad y el bienestar de los pacientes.
La psicoterapia asistida con ketamina, integrada con técnicas cognitivo-conductuales, ofrece un enfoque innovador y respaldado por evidencia para la salud mental en Uruguay y en el mundo.
Su éxito depende de la capacitación adecuada de los profesionales, la claridad en los roles y el acompañamiento constante de los pacientes.
- Schedule Psychedelic Telehealth Programa Psicodélic Telesalud
- Contact Contacto
- About Acerca de
- Publications Publicaciones
Una visión evolutiva de la terapia cognitiva conductual en la psicoterapia asistida por psicodélico moderna y la terapia psicodédicia y la ketamina Véase la revisión preliminar de la página de más fuentes y resúmenes (Ediciones en curso)
En los debates de política sobre medicamentos psicodélicos, la psicoterapia asistida por psicodélico y las diversas funciones de los proveedores, los alcances de la práctica y las competencias con todos sus matices pueden no ser abordados, o se desestiman sumariamente por no estar basados en pruebas y demasiado difíciles de estudiar.

August 2025: "A carefully controlled dose of ketamine (a dual anaesthetic and painkiller medicine that affects certain brain receptors) given by drip, and a course of cognitive behavioural therapy, or CBT, designed to specifically help prevent relapse shows promising results - In phase II testing, people given the treatment had 50 per cent fewer heavy drinking days compared to those who received a placebo."

""La ketamina modulador glutamatoérgico ha creado un plan para estudiar nuevos productos farmacéuticos en el campo. Estudios recientes sugieren que los psicodérgicos serotonérgicos (SP) clásicos también pueden tener eficacia antidepresiva. Tanto la ketamina como los SP parecen producir efectos antidepresivos rápidos y sostenidos después de un período psicoactivo transitorio. (2020)”
La terapia conductual cognitiva es un conjunto de conceptos que un psicoterapeuta puede ayudarle a aprender a aplicar en su salud mental en curso. Los psicoterapeutas tienen licencia para trabajar con estos conceptos con individuos y grupos en persona, en casa, en hospitales, iglesias, sitios de desastre, en la naturaleza o a través de la telesalud.
A veces la medicina se añade a la psicoterapia como lo indica un proveedor de atención médica, con algunos medicamentos que caen bajo el término de la medicina psicodélica, que incluye ketamina rastrera, un medicamento genérico fuera de patente originalmente aprobado por la FDA en 1970, y utilizado como medicina anestésica en dosis altas. La ketamina está en la lista de Medicamentos Esenciales de la OMS, y ha sido estudiada simultáneamente en dosis sub-estéticas, pero totalmente psicodécicas desde 1970, para una serie de indicaciones de salud mental, incluyendo ansiedad, depresión, alcoholismo, manejo del dolor y TEPT. Como un medicamento reutilizado con más de 60 años de uso clínico, la ketamina se ha estudiado durante una serie de indicaciones más que muchos medicamentos psiquiátricos aprobados por la FDA aprobados para uso doméstico diario. Esta revisión de la literatura tiene como objetivo, a través de la investigación, integrar algunas de las partes dispares de la atención de la salud mental, que ahora incluye medicamentos psicodélicos y una cierta desilusión con las industrias psiquiátrica y farmacéutica, ya que estos medicamentos se normalizan como opciones viables y modernas de atención de salud mental.

Diferentes medicamentos requieren preparación y soporte específicos
Hay varias necesidades que tiene un cliente cuando trabaja con medicamentos que afectan la salud mental y el bienestar. Todos los medicamentos, incluidos los antidepresivos tradicionales como los SSRI, vienen con precauciones, riesgos y expectativas sobre la mejor manera de apoyar la mejor manera de que ese medicamento funcione. Una compañía farmacéutica promovió la idea con una caricatura de que la depresión es causada por no suficiente serotonina, aunque estudio reciente sugiere que no es el caso. Vargas y colegas escriben en 2023, en su estudio "Los psicodélicos promueven la neuroplasticidad a través de la activación de los receptores intracelulares 5-HT2A":
“La serotonina, debido a su composición química polar, no puede pasar fácilmente la membrana de células neuronales. La serotonina no induce la plasticidad. Por lo tanto, aumentar los niveles de serotonina mediante inhibidores selectivos de la recaptación de serotonina (ISRS) fue en gran medida un esfuerzo inútil para el tratamiento significativo de la depresión. Sólo una pequeña porción de los pacientes responde.”
Otra forma de prepararse para un medicamento es comprender el riesgo de efectos secundarios que pueden considerarse adversos. Este estudio "Efectos secundarios de los antidepresivos durante el uso a largo plazo en un entorno naturalista (Bet, et al, 2013) encontró:
"Los efectos secundarios de los antidepresivos generalmente no se reportan suficientemente en ensayos clínicos y los estudios naturalistas a gran escala se limitan a seis meses de uso. Examinamos la prevalencia y la naturaleza de los efectos secundarios percibidos por el paciente y sus determinantes durante el uso antidepresivo a largo plazo en un entorno naturalista. Los sujetos, de 19 a 67 años, en el Estudio de Depresión y Ansiedad de los Países Bajos fueron contratados en atención primaria y la atención especializada en salud mental abarcó 927 casos de uso único de antidepresivos. En el 64% de los casos, en promedio, se reportaron 2.9 efectos secundarios... Mostramos que el efecto secundario antidepresivo, conocido por estudios a corto plazo, persiste durante el uso a largo plazo y se asocia con severidad de la depresión y la dosis de antidepresiva. Un hallazgo novedoso fue que la venlafaxina está asociada con una sudoración más profusa y ese aumento de peso parecía más específico en las usuarias. Los médicos deben ser conscientes de que, durante el uso antidepresivo a largo plazo, los efectos secundarios son comunes y persistentes."
La ketamina racial, un medicamento genérico aprobado por la FDA actualmente disponible en todo el mundo, ha sido estudiado durante más de 60 años. Este medicamento se describe como psicodélico (disociativo, disuelto de ego, fuera del cuerpo) y/u otros efectos visionarios, que requieren precauciones y soporte, pero diferente de una SSRI. Este medicamento ha sido categorizado como un anestésico disociativo, y está aprobado por la FDA en humanos y animales para la anestesia y sedación. Se ha estudiado y recetado fuera de la etiqueta desde 1970 para una serie de indicaciones de salud mental y dolor.
En gran parte de la literatura, el efecto disociativo", otra palabra para psicodélica, a veces se considera un efecto adverso. El apoyo y las precauciones relativas a la ketamina van desde muy poco cuidado con la dosis muy baja de ketamina recetada desde proveedores médicos con un punto de vista, hasta que la ketamina se administra por bomba intravenosa o goteo directamente a su torrente sanguíneo mientras está bajo observación médica. Los enfoques corren la gama.
Cuando un medicamento se administra en el torrente sanguíneo por inyección puede tener un nivel elevado de riesgo, lo que requiere una monitorización continua en comparación con la ingesta del medicamento por vía oral. Por ejemplo, la benzodiazepina (Valium) por inyección, vs por vía oral, que ha permitido recetar benzodiacepinas para el uso doméstico, aunque en dosis más altas estos medicamentos también se utilizan para "inducir la relajación y causar amnesia antes de las operaciones quirúrgicas. Estos medicamentos también se recetan para indicaciones de salud mental como ansiedad. De la FDA:
Revisamos las bases de datos de poscomercialización, los casos de eventos adversos reportados a la FDA* y la literatura publicada sobre abuso, uso indebido, adicción, dependencia y abstinencia asociada con el uso de benzodiazepina (ver Resumen de datos). Nuestra revisión encontró que las benzodiacepinas son ampliamente prescritas en los EE.UU., a menudo por largos períodos de tiempo. También son ampliamente abusados y mal utilizados, a menudo junto con el alcohol, los opioides recetados y las drogas ilícitas, que empeoran los riesgos de problemas graves. También encontramos que algunos pacientes han tenido reacciones graves de abstinencia después de que las benzodiacepinas se detuvieron repentinamente o la dosis se redujo demasiado rápidamente. Algunos pacientes experimentaron síntomas de abstinencia que duraron muchos meses.
En "La ketamina no paternaria para la depresión: una discusión práctica sobre el potencial de la adicción y recomendaciones para la prescripción juiciosa" (Swainson, et al, 2022), los investigadores informan:
La ketamina intravenosa (IV) se usa cada vez más fuera de etiqueta a dosis subanestéticas por su rápido efecto antidepresivo, y la esketamina intranasal (IN) ha sido aprobada recientemente en varios países para tratar la depresión. La utilidad clínica de estos tratamientos está limitada por la escasez de programas de ketamina IV y de esketamina IN financiada con fondos públicos y barreras de costos para los programas de tratamiento privado, así como el costo de la propia droga para la propia esketamina IN, que hace que las alternativas genéricas de ketamina sean una opción atractiva. Aunque la evidencia es limitada, el uso de formulaciones de ketaminas corredátricas no parentales (oral, sublingual e IN) puede ofrecer un acceso más realista en entornos menos rígidamente supervisados, tanto para el tratamiento agudo como para el mantenimiento en casos selectos. Sin embargo, la literatura psiquiátrica ha advertido repetidamente sobre el potencial adictivo de la ketamina y ha levantado la cautela tanto para el uso de ketamina menos supervisado como a largo plazo. Hasta la fecha, estas preocupaciones no se han discutido en vista de la evidencia disponible, ni se han discutido en un contexto clínico más amplio. Este trabajo examina la literatura pertinente disponible y sugiere que los riesgos de uso indebido de ketamina no parecen diferentes a los de otros agentes bien establecidos y comúnmente prescritos con potencial de abuso, como estimulantes o benzodiacepinas. Como tal, la prescripción de ketamina debe considerarse en un contexto similar de riesgo/beneficio para equilibrar el acceso de los pacientes y la necesidad de tratamiento con preocupación por el posible uso indebido de sustancias. Nuestro consorcio de especialistas en trastornos del humor con experiencia significativa en receta de ketamina considera la prescripción de ketamina no paterna una opción de tratamiento clínico razonable en casos selectos de depresión resistente al tratamiento. Este artículo describe dónde esto puede ser apropiado y hace recomendaciones prácticas para los médicos en la prescripción juiciosa de ketamina no parental.
Hay riesgos conocidos. El tratamiento implica planificar con anticipación disminuir cualquier probabilidad de daño, y para maximizar la posibilidad de que el medicamento ayude en su curación y disminuya el sufrimiento. La ketamina administrada por vía oral en el rango subanestésico clasificado al cliente individual puede ser vista por los proveedores médicos especializados en ketamina como un nivel aceptable de riesgo para que sus pacientes tomen en casa para una serie de dolor fuera de etiqueta e indicaciones de salud mental, como se evidencia en el estudio científico en curso y la práctica aceptada en la atención médica y mental, especialmente cuando se apoya la psicoterapia cognitiva conductual.


Spravato is given to assist a new antidepressant regimen, and not in conjunction with cognitive behavioral therapy.
Clarification of Roles
Research continues to show that ketamine, like serotonergic psychedelic medicines, may elicit a psychedelic experience, which may be an important factor in treatment. This approach involves a multidisciplinary team.
- Proveedor médico / Psiquiátrica / Prescripción Clinicia: Encargado de evaluar y diagnosticar su condición y recetar un curso de tratamiento que puede incluir un medicamento que afecta su salud mental de alguna manera. Ese medicamento, mientras esté en su cuerpo, puede tener efectos agudos, como en el caso de la ketamina. Los proveedores médicos trabajan en oficinas y clínicas, así como a través de la telesalud. Estos proveedores pueden optar por recetar un medicamento "off-label" si tienen suficientes razones clínicas para que pueda ayudar a una población clientelar, como aquellos que tratan con síntomas de salud mental como ansiedad o depresión. El proveedor médico ofrece un marco de diagnóstico médico y psiquiátrico, prescribiendo un tratamiento de medicina y el nivel de seguridad requerido. La ketamina por vía oral tiene antecedentes de ser autoadministrada fuera de una clínica, mientras que la ketamina a través de la inyección, iv o intranasalmente puede tener un nivel de riesgo creciente que su proveedor médico puede sentirse mejor en un entorno médico. El reembolso de los seguros suele ser posible sólo con las indicaciones aprobadas por la FDA. Spravato, el nombre de marca para la mitad de la molécula de ketamina, esketamina, es prohibitivamente caro para muchos por sí solo, y no se ha demostrado que sea superior a la ketamina racial genérica, que ya está ampliamente disponible en farmacias con licencia en todo el mundo. Spravato también se prescribe como tratamiento crónico, además de iniciar un nuevo antidepresivo diario, también un tratamiento crónico, y con su propio conjunto de riesgos psicológicos y fisiológicos.
- Proveedores de Salud Mental con licencia: Se trata de médicos capacitados para evaluar y tratar las condiciones de salud mental. Con una formación avanzada en la aplicación de un medicamento o un conjunto de medicamentos a la salud mental y el bienestar de la persona, médicos de salud mental como el matrimonio y los terapeutas familiares (LMFT's), los consejeros clínicos (LPC, LMHC), los trabajadores sociales clínicos (LCSW), los profesionales de enfermería (NP) o sus homólogos doctorales, como los psicólogos clínicos (PsyD) apoyan lo que un medicamento está haciendo agudamente en el cuerpo (mente/cerebro), así como apoyar al cliente en una relación continua y profesional en el ámbito de la práctica y las competencias exclusivas del proveedor. Esta práctica, generalmente llamada consejería de salud mental o psicoterapia, existe dentro de la actual estructura médica aceptada en los EE.UU. y la mayoría de los demás países. Esto se ha hecho históricamente en la oficina terapeuta, en la casa de un cliente, en una iglesia o templo, campamento de locura, escuela, hospital, etc. Los profesionales de la salud mental con licencia pueden tener experiencia trabajando con SSRI, ciertos grupos de edad o poblaciones, terapia asistida con animales, medicamentos psicodélicos, terapia sexual, trastornos del consumo de sustancias o cualquier otro tipo de subespecialidades. Los médicos de salud mental con licencia tienen experiencia práctica trabajando en estas áreas durante las pasantías de entrenamiento de posgrado y prácticas en el nivel de maestría, así como 3000 o más horas clínicas supervisadas después de la escuela de posgrado (similar a una residencia médica) antes de ser licenciada de forma independiente, lo que requiere aprobar conocimientos y exámenes de ética, y ser tomados las huellas dactilares. Después de tener licencia, se requiere educación continua tanto para mantener la licencia, como para mantener éticamente un nivel de competencia en las áreas de práctica de la terapeuta de salud mental. Colorado está empezando a ofrecer certificaciones clínicas de facilitador psicodélico para especialistas en salud mental. En todo el mundo, los proveedores de salud mental con licencia proporcionan psicoterapia asistida por medicamentos como ketamina, SSRI, enutectogenes, antidepressantes, medicamentos contra la ansiedad, neuroplastógenos y/o medicamentos para plantas, y lo hacen competentemente cuando se capacitan, ya que se encuentran nuevos medicamentos eficaces en condiciones de salud mental.
- Facilitador psiquiátrico (Guía, Coach, Doula, carrocería, etc.): Esta persona puede ser adicional a un psicoterapeuta, y puede o no hacer una integración continua como parte del tratamiento de salud mental. Pueden ser muy beneficiosos en otras formas del cuerpo, la mente, el corazón y el espíritu, y apoyar a un cliente de forma segura a través de cualquier experiencia de medicina que puedan tener, pero un facilitador psicodélico puede ser un apoyo adicional durante la experiencia de la medicina aguda. Un facilitador psicodélico puede ser un chamán, yogui, curandera, masajista, fisioterapeuta, u otro tipo de trabajador del cuerpo, capellán, doula de la muerte, o quienquiera que sea el cliente puede sentirse cómodo y seguro con el tiempo que se le ocurre sobre los efectos agudos de un medicamento. El facilitador se sienta con la persona en su casa, en la oficina, en un retiro, hospicio, en la naturaleza, o en una ceremonia, dependiendo de la medicina y la ruta de la administración. Un facilitador psicodélico no es un profesional de la salud mental con licencia, y su papel no es diagnosticar, evaluar o tratar un diagnóstico de salud mental. El facilitador puede o no tener contacto continuo con el cliente fuera de la experiencia de la medicina aguda. Oregon tiene una licencia de facilitador psicodélico. Colorado también está empezando a ofrecer una licencia de facilitador no clínica. Otros estados están en conversaciones para comenzar a certificar a los facilitadores que no tienen licencia de médicos. Una certificación de facilitador psicodélico no es lo mismo que una licencia para proporcionar servicios de salud mental como la psicoterapia.

La ketamina es un medicamento legalmente disponible que los proveedores médicos reutilizan para su uso en indicaciones fuera de la etiqueta. La legalidad local de diferentes moléculas, quién puede ingerir estas sustancias, y bajo qué guía puede variar según su ubicación y situación particular.
El sexo no es parte de esta relación, con ningún miembro de un equipo de tratamiento psicodélico.

La psicoterapia asistida por ketamina con un especialista en salud mental altamente entrenada implica aprender y aplicar un conjunto de conceptos, como la terapia cognitivo-conductual, para apoyar las nuevas conexiones neuronales y nuevas formas de pensar que acompañan el tratamiento exitoso con este medicamento, que se ha descrito de manera similar a medicamentos como MDMA, DMT, LSD, 5-MEO-DMT, ibogaine, psilocybin, psilocina, arketamina, esketamina, r-MDMA, y otros. Muchos de estos medicamentos están abriéndose paso a través del proceso de aprobación de la FDA, patrocinado por varias corporaciones farmacéuticas.
Psicoterapia asistida con ketamina: Revisión sistemática de la literatura (Drozdz, et al, 2022)
"El uso de Psicoterapia Asistida de Ketamina (KAP) puede potencialmente satisfacer la necesidad clínica no satisfecha de un tratamiento eficaz para múltiples trastornos complejos y a menudo concomitantes de dolor, psicológico y consumo de sustancias. La pseutrófia demostró su capacidad para producir efectos antidepresivos y ansiolíticos probablemente interactúe con los procesos involucrados en la psicoterapia, idealmente como un conducto para un cambio rápido, aumentando el compromiso y la adherencia del tratamiento, construyendo la alianza terapéutica y reduciendo la defensividad proporcionando repudios de la symptomología angustiosa mientras induce experiencias transpersonales a dosis más altas. El continuo compromiso en la psicoterapia después de la administración de la ketamina puede prolongar los efectos a menudo transitorios de la ketamina y permitir la integración de la perspicacia psicológica en el funcionamiento cotidiano. Si bien en la actualidad no existe un enfoque estándar para la aplicación de la KAP, es importante preparar y apoyar al paciente durante la administración de la ketamina y ofrecer sesiones de psicoterapia de seguimiento para mantener efectos positivos y retrasar o eliminar la recaída. A medida que la investigación de KAP continúa evolucionando, un enfoque en aumentar la duración de los efectos positivos puede conducir a intervenciones y programas de mantenimiento eficaces, mejorando el KAP de manera que se convierta en un tratamiento eficaz y duradero para condiciones complejas, resistentes y crónicas para las personas que viven con trastornos del dolor, la salud mental y el consumo de sustancias".
On dosing escalation / exploration / titration:
"The theorized effectiveness of ketamine in psychotherapy is based on: (a) increased acss to traumatic memory via enhanced synaptic connectivity; (b) decreased central sensitization via downregulation of the prefrontal cortex, and (c) enhanced extinction of previously paired pain-related memories.21 Therefore, KAP can utilize a dosage escalation strategy to achieve different levels of trance, increasing to full out-of-body experiences.23")
In a psychotherapy model, the therapist and client develop a plan for the client’s ongoing mental health and quality of life, curating the therapeutic process to create a container and therapeutic alliance in which to explore what comes up for the client in the process.
Psychedelic therapy historically involves talking to a mental health provider before, usually during, and after each medicine administration, especially initially. Integration psychotherapy sessions are generally within a few days of a medicine session. Clients may go on to make sense of their journey in ongoing counseling as needed, in addition to body work, yoga, or other pursuits that may be beneficial to individual mental health.

"Perhaps, rather than trying to rid psychedelic therapy trials of all human interaction in order to better isolate the effect of drug administration, thereby maximizing pharmaceutical and insurance control over who can access this treatment, we should instead acknowledge the limitations of this particular form of knowledge formation and use other means to discern best practices. Intuition, clinical judgement, and an appreciation for the thousands of years of history surrounding the use of psychedelic drugs could be a good start."

Systematized Review of Psychotherapeutic Components of Psilocybin-Assisted Psychotherapy (Horton, et al, 2021)
The bedrock of PAP rests on providing nonjudgmental listening, empathic support, and a strong therapeutic relationship (1, 2, 24). Although the PAP studies in this review have largely been conducted and published within the domain of psychiatry (4, 10, 14), and may thus seem distant from the world of therapists, the fundamental components of PAP are integral to nearly every model of psychotherapy. Moreover, the therapists in the reviewed clinical trials were often not psychiatrists, but master’s level counselors (N=7), social workers (N=8), and clinical psychologists (N=19). This finding suggests that, if PAP becomes a clinical practice, the individuals who will work directly with clients before, during, and after psilocybin administration will likely be practicing therapists. Clinicians may be able to incorporate their preexisting knowledge and skills along with specific training in PAP to help facilitate immediate and enduring positive changes in the lives of their clients.
...
The present systematized review outlined the role of therapists in PAP and consolidated the structure of sessions and range of psychotherapeutic modalities and techniques implemented in this therapy. The importance of isolating psilocybin’s effects to better understand its mechanistic functions is unquestionable. Additionally, the content of each stage of PAP is essential to the efficacy of psilocybin treatment, and the influence of psychotherapy on outcomes is likely higher than current research suggests (2). Counselors and therapists are poised to contribute immensely to the field of PAP, as they will likely provide the in-session therapeutic services if or when psilocybin becomes an FDA-approved treatment.
Increasing Access through Telehealth
"At-Home Ketamine" is being prescribed by medical providers who view the medicine as the catalyst for your healing. Sometimes these providers work for companies charging a high price for generic medication that is widely available in licensed compounding pharmacies around the world. Some of these providers view mental illness as a chronic disease where something is wrong in your body for which they believe ongoing medication is required. Other providers are prescribing doses of ketamine that may have an experiential component without the licensed mental health support trained and experienced in dealing with the emotions and behaviors of individuals and groups. The experience, indeed considered an adverse effect in many studies, is considered by psychedelic practitioners to be a feature of the process. Psychedelic practitioners
Psychotherapists working remotely use modern tools to connect with clients beyond the confines of a medical office, tending to privacy and safety needs as appropriate. Ketamine by mouth has been prescribed to self-administer for decades, and has been studied in repeat use in humans for as long as 18 years. Some humans are susceptible to bladder issues, heart issues, psychiatric issues, or find ketamine to be something easily misused.

Consider Hull, et al, in 2022 in their study "At-home, sublingual ketamine telehealth is a safe and effective treatment for moderate to severe anxiety and depression: Findings from a large, prospective, open-label effectiveness trial", concluding:
At-home KAT response and remission rates indicated rapid and significant antidepressant and anxiolytic effects. Rates were consistent with laboratory- and clinic-administered ketamine treatment. Patient screening and remote monitoring maintained low levels of adverse events.
This research was expanded in a longitudinal study by Mathai, et al, 2024 "At-home, telehealth-supported ketamine treatment for depression: Findings from longitudinal, machine learning and symptom network analysis of real-world data”.
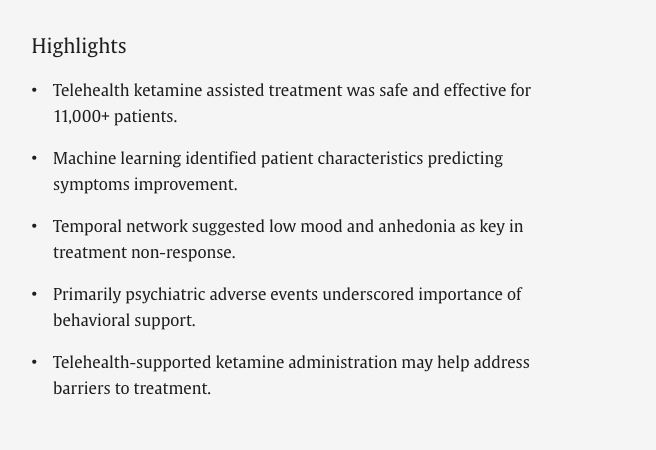

A sample of 11,441 patients was analyzed, demonstrating a modal antidepressant response from both non-severe (n = 6384, 55.8 %) and severe (n = 2070, 18.1 %) baseline depression levels. Adverse events were detected in 3.0-4.8 % of participants and predominantly neurologic or psychiatric in nature. A second course of treatment helped extend improvements in patients who responded favorably to initial treatment. Improvement was most strongly predicted by lower depression scores and age at baseline. Symptoms of Depressed mood and Anhedonia sustained depression despite ongoing treatment.
...
At-home, telehealth-supported ketamine administration was largely safe, well-tolerated, and associated with improvement in patients with depression. Strategies for combining psychedelic-oriented therapies with rigorous telehealth models, as explored here, may uniquely address barriers to mental health treatment.

July 2024: “As some patients will inevitably resist discharge to a telehealth service and/or a new provider, academic ambulatory programs will need to develop structural methods for clearly communicating this model to patients from the outset of treatment,” the authors say. “Furthermore, long waitlists—frustrating to patients and referring clinicians alike—could be shortened by identifying patients who are unlikely to require academic resources and triaging these individuals directly to telehealth companies.”
When working with ketamine by mouth (oral or sublingual), the effects are much less sudden than IV-administered ketamine, and studies continue to show that there can be an experience (described in the literature as dissociation, emergence phenomenon, psychotomimetic, psychedelic). Although considered sometimes as an Adverse Effect, research suggests most people find any unwanted experience or effects were minimal and short-lived, and find the resulting benefits to be noticeable and substantial. The acute effect, depending on the dose and route of administration ranges from 1-3 hours, and which may feel like a deep meditation. For many suffering with pain, stress, burnout, addiction, anxiety and depression, even suicidality, the positive effects may be noticeable within 1-2 hours, and may be sustained with further human support, specifically someone trained in cognititve behavioral therapy as part of a robust, experiential psychedelic practitioner training and mentorship program.
Having a sober adult around to take care of you if anything comes up, or who can call for help if you needed medical attention is a way to decrease the risk of misusing the medicine in a way that may lead to harm.
Here is Tsang, et al, in 2023 "Safety and tolerability of intramuscular and sublingual ketamine for psychiatric treatment in the Roots To Thrive ketamine-assisted therapy program: a retrospective chart review”:
These findings suggest good safety and tolerability for RTT-KaT among individuals seeking treatment for mental health issues. The majority of participants did not experience adverse reactions and the adverse events that were recorded involved transient symptoms that were resolved with rest and/or medications. The group therapy model described provides a comprehensive approach and presents a promising model for operating a KaT program in a community setting.

In person, or via telehealth, the mental health provider monitors the client while under the acute effects of the medicine. In the case of telehealth, the psychotherapist may ask a client to provide an adult Emergency Contact to be a sober sitter during the medicine session, checking in periodically on their safety. In the unlikely case of emergency, both the sober sitter and/or the therapist would contact 911 and the medical provider, as would happen in a psychotherapist's office, retreat setting, or psychiatry clinic. In tandem with the sober sitter, the therapist sees the dose the client is taking, how they administered it, and is monitoring what comes up for the client to integrate in subsequent psychotherapy sessions. Progress in psychotherapy may be reported to the medical provider before clients receive further refills on the medicine. The psychotherapist may ask the client to take a beginning and ending blood pressure as a cognitive behavioral intervention in relaxation to tend to helping the client prepare their inner experience. Music and eyeshades are also tools used in research and practice, to minimize outside distraction. A cognitive behavioral therapist views these as behavioral interventions to promote relaxation and openness to having an experience with the medicine that feels healing, as opposed to it feeling like a “Serious Adverse Event” (SAE). Cognitive-behavioral therapy is a secular mindfulness approach that allows for helping clients to contain the experience of being human, including the experiences when working with psychedelic medicines like ketamine in the sub-surgical / sub-anesthetic dose.
Finding Our Lanes: A Roadmap for Collaboration Between Academic Medical Centers and Behavioral Telehealth Companies (Eden, et al, 2024):
"A roadmap for strategic integration is presented for how academic centers-institutions frequently overwhelmed by patient volume-might leverage partnerships with a private sector eager to utilize novel technology to improve access, demonstrate data-driven outcomes, and advocate for improved reimbursement from payers. We also assess the potential risks and pitfalls of such collaboration. In return, academic institutions can refocus on their strengths, including research, systems knowledge, quality-improvement initiatives, education and training, and specialty clinical care."
In "Music as an Intervention to Improve the Hemodynamic Response of Ketamine in Depression— A Randomized Clinical Trial”, researchers Greenway, et al, (2024) write:
Beyond psychiatric contexts, the stimulatory hemodynamic effects of ketamine have received extensive study, both as desirable (eg, in surgical contexts) and as potentially harmful (eg, in procedural sedation),5 but never in relation to music, to our knowledge. The magnitude of the hemodynamic effects observed in this study suggests that ketamine research should consider potential influences of contextual factors, including auditory stimuli. Ketamine’s unique psychoactive effects may amplify the effects of music and other environmental influences, as has been long observed in the anesthesiology literature.
Ketamine-assisted psychotherapy, facilitated remotely, with ongoing support and a sober sitter available during the acute effects of the medicine, taken by mouth (or suppository) is a possibility for some clients. For others, a higher level of medical intervention during the acute medicine stage may be advised by your medical provider, with patients following up with a psychotherapist in-person or via telehealth in the days before and following the medicine administration. For clients with additional comorbidities, in-patient options may be more appropriate.
There are many tools a psychotherapist may use to help clients learn to speak the language of cognitive behavioral therapy, especially tools which may help facilitate a therapeutic alliance, including, but not limited to telehealth. While some medicines may be deemed by your medical provider as safe for use outside of a clinic setting, psychotherapists may offer services throughout the state in which they're located via telehealth, in addition to whatever local, in-home, or in-office, or in-patient support they may provide, as indicated in the scopes of their mental health practitioner license.
In the article "Using Telehealth to Implement Cognitive-Behavioral Therapy” (Dent, et al, 2018), researchers write:
Therapists are required to be experienced in cognitive-behavioral therapy, adept at telehealth care delivery, and knowledgeable about the care of high-risk populations with general medical conditions and behavioral health issues or who are navigating life transitions.
...
"Behavioral health conditions are prevalent among patients with medical comorbidities and often go unrecognized or untreated because of barriers, including inadequate identification of patients in need and insufficient access to high-quality behavioral health care. We have described a nationally scaled telehealth model designed to overcome barriers to identification and enrollment into therapy. Participants were highly satisfied and experienced clinically meaningful improvements in behavioral health outcomes, further underscoring the potential impact that a telehealth solution could have in optimizing treatment outcomes."
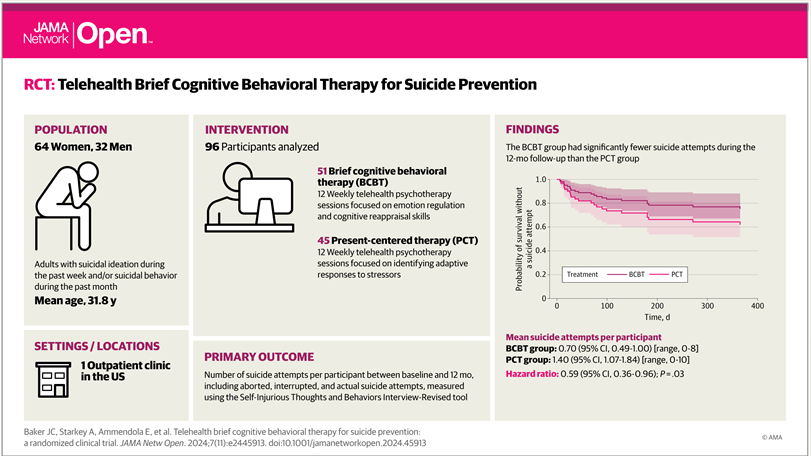
In 2024, JAMA reported in "Telehealth Brief Cognitive Behavioral Therapy for Suicide PreventionA Randomized Clinical Trial (Baker, et al):
Results of this randomized clinical trial of 96 US adults with recent suicidal ideation and/or suicidal behavior show that patients who received BCBT had significantly fewer suicide attempts during the 1-year follow-up vs patients who received present-centered therapy. Reductions in suicidal ideation occurred in both treatments with no significant differences between groups.
These findings suggest that BCBT delivered via video telehealth is effective for reducing the risk of suicide attempts among adults with recent suicidal ideation and/or suicidal behavior.

These are some of the nuances that are often missed in the larger discussions among policy makers as they decide for the rest of us how to roll out a powerful medicine without getting hooked on it, yet consuming of it to fuel capitalism. There is not much money to be made, comparatively, in small private practices offering quality integrated care, charging for their time and overhead to work with the least amount of generically available medicine the most effectively. Ketamine-assisted psychotherapy, whether in a therapist's office or at home, has been shown to help people suffering with a number of indications considered "off-label". FDA-approved as an anesthetic in 1970, racemic ketamine has been administered, at least once, to billions of people (Billions!) around the world, across age and disease spectrum, in clinics, homes, and on battlefields. Over 5000 studies on ketamine and depression add to the decades of study on cognitive behavioral therapy (over 61,000 results on pubmed) and over 100 years of study of psychedelic medicine experiences as being adjunctive to psychotherapy. It takes several million dollars to take a medicine through the FDA-approval process, limiting the FDA approval of off label medicines such as ketamine, psilocybin, LSD, MDMA, DMT, and other generically available, off-patent molecules that have been studied in conjunction with psychotherapy for over a century.
In 2024’s "Ketamine-assisted psychotherapy, psychedelic methodologies, and the impregnable value of the subjective—a new and evolving approach" Wolfson & Vaid, write:
The ketamine session provides therapeutic impact along many different axes. An experience of safety and defensive softening permits deeper contact with feeling states and aspects of the self that previously needed to be disconnected from for emotional survival. Reconnecting with these disavowed states and self-aspects in a field of safety and relational care allows for trauma metabolism and release that heals early wounds and integration through reconnection contributing to integrity and resilience. New insights and knowledge are frequently accessed both during and after sessions. Navigation of the ketamine experience cultivates the platform of an awareness state—a new or revived witnessing of one’s self—such as new views and attitudes, reframing, connection, affection and love, improvement in reality testing and sensitivity to the body and its sensations and states. The ‘letting go’ increases our capacity to notice and observe the symphony of qualia, the great show of being alive and sensate, interdependent, and connected, fostering mindfulness and loving kindness toward self, others and rooted in nature.
Fear-based media reports a "proliferation" of ketamine clinics, which is a distorted way of describing increased access to healthcare. Quality treatment incorporates modern approaches to human connection, that may include working with a medicine in addition to human-to-human psychotherapy. The minimum standards of mental health and medical practice are locally regulated, and local practitioners meeting these standards are able to specialize in ketamine-assisted treatments.
Regardless of the level of standards and quality of service, even evidence-based care and support includes a risk of failing to meet the needs of 100% of patients. As with any mental health approach, we understand a human may go on to feel miserable after a treatment, even to the point of harming themselves or others. A mental health professional cannot "save" anyone. Psychotherapists offer a set of mind-body concepts as a small way to reduce suffering. This helps a great deal of people. Others will go on to hurt themselves or someone else. Still others are or have been harmed by psychotherapists or other helper professionals, spiritual guides, or medical prescribers, or have had negative reactions to a medicine, all of which are known risks being studied in ongoing research.

Some Historical Context to “Assisted-Psychotherapy"
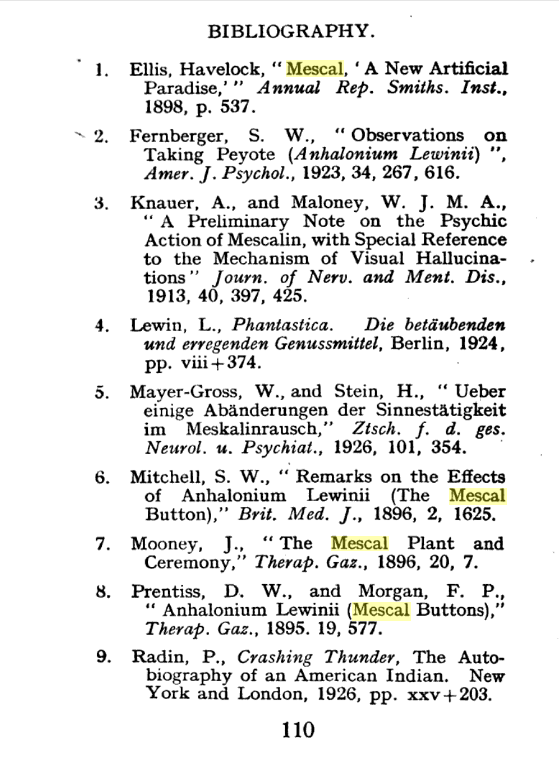
In The Encounter That Introduced Peyote to Western Science, researchers describe John Mooney’s 1893 experience on peyote written up in the 1896 Therapeutic Gazette and cited in this bibliography from 1928, which cites research throughout the early 1900’s. Merck first synthesized MDMA in 1912, and Parke, Davis synthesized ketamine in 1962, comparatively.
Mooney took the peyote back to Washington DC, where he gave around half of the buttons to the chemistry division of the Department of Agriculture, and another batch to the medical department of Columbian (now George Washington) University. By this time, a few Western doctors and cactus traders had heard tales of peyote’s wonderful properties and purchased samples from the peyoteros who supplied it around the Texas-Mexico border, and the Detroit pharmacists Parke, Davis were developing a mild tincture as a cardiac stimulant. But its visionary and spiritual powers were still unexplored by Western science. Columbian’s professor of materia medica, Daniel Webster Prentiss, used the buttons Mooney supplied to conduct the first scientific trials.
In 1897, after reading Mitchell’s article, the German chemist Arthur Heffter made a series of self-experiments with peyote extracts and isolated the compound that was responsible for the visual hallucinations: an alkaloid that he named “meskalin.”
Modern psychotherapy developed in the late 1800’s with cognitive behavioral therapy studied since the 1950’s. Whether delivered at home, via telehealth, or in person, CBT continues to be show a strong signal of efficacy for a number of indications, and must be considered alongside psychedelic medicine in research and practice. Additionally, the results of CBT are measurable by observable differences in the brain as evidenced on fMRI.
In the Dunlop, et al, 2017 paper "Functional Connectivity of the Subcallosal Cingulate Cortex And Differential Outcomes to Treatment With Cognitive-Behavioral Therapy or Antidepressant Medication for Major Depressive Disorder”, researchers write:
“Remission from major depression via treatment with CBT or medication is associated with changes in rsFC (resting state functional connectivity) that are mostly specific to the treatment modality, providing biological support for the clinical practice of switching between or combining these treatment approaches. Medication is associated with broadly inhibitory effects. In CBT remitters, the increase in rsFC strength between networks involved in cognitive control and attention provides biological support for the theorized mechanism of CBT. Reducing affective network connectivity with motor systems is a shared process important for remission with both CBT and medication.”
In the meta-analysis spanning over 20 years of psychotherapy research "A systematic review and meta-analysis of transdiagnostic cognitive behavioural therapies for emotional disorders" (Schauffele, et al, 2024) researchers state:
Transdiagnostic cognitive behavioural psychotherapy (TD-CBT) may facilitate the treatment of emotional disorders. Here we investigate short- and long-term efficacy of TD-CBT for emotional disorders in individual, group and internet-based settings in randomized controlled trials (PROSPERO CRD42019141512). Two independent reviewers screened results from PubMed, MEDLINE, PsycINFO, Google Scholar, medRxiv and OSF Preprints published between January 2000 and June 2023, selected studies for inclusion, extracted data and evaluated risk of bias (Cochrane risk-of-bias tool 2.0). Absolute efficacy from pre- to posttreatment and relative efficacy between TD-CBT and control treatments were investigated with random-effects models. Of 56 identified studies, 53 (6,705 participants) were included in the meta-analysis. TD-CBT had larger effects on depression (g = 0.74, 95% CI = 0.57–0.92, P < 0.001) and anxiety (g = 0.77, 95% CI = 0.56–0.97, P < 0.001) than did controls. Across treatment formats, TD-CBT was superior to waitlist and treatment-as-usual. TD-CBT showed comparable effects to disorder-specific CBT and was superior to other active treatments for depression but not for anxiety. Different treatment formats showed comparable effects. TD-CBT was superior to controls at 3, 6 and 12 months but not at 24 months follow-up. Studies were heterogeneous in design and methodological quality. This review and meta-analysis strengthens the evidence for TD-CBT as an efficacious treatment for emotional disorders in different settings.
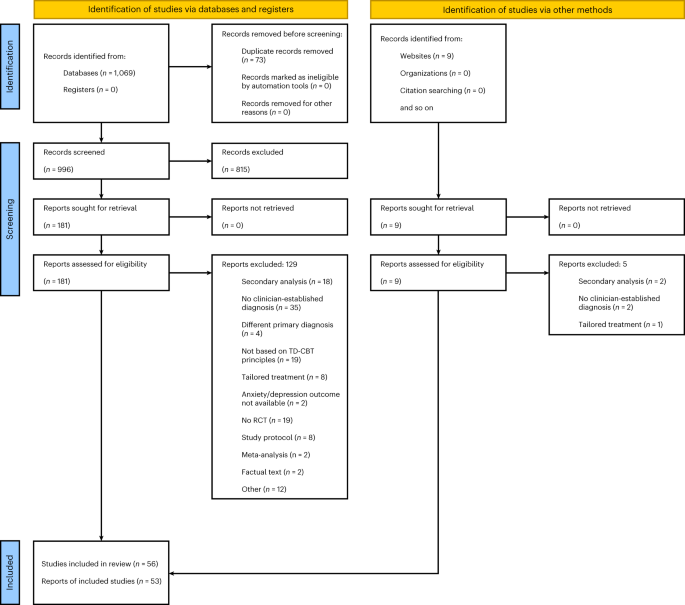
In comparing 53 different studies on psychotherapy, these researchers conclude that what they found “strengthens the evidence of transdiagnostic cognitive behavioral therapy psychotherapy is efficacious for treatment of emotional disorders in different settings”, including by “internet-based settings”, ie, telehealth. Trans-diagnositic cognitive behavioral therapy approach, and generalizable, standardized and evidence-based practice was better than nothing at all (being on a “waitlist”), and at least as effective to active treatments for anxiety (medicine) and superior, that is, more effective than “other active treatments for depression”. This generalizable model, even by internet-based means of delivery, was comparable to styles of cognitive behavioral therapy that focus on a particular type of unhealthy negative emotion, feeling or behavior pattern.
Rational emotive behavior therapy (REBT), introduced by Albert Ellis in the late 1950s, is one of the main pillars of cognitive-behavioral therapy...REBT is a sound psychological intervention.
50 years of rational-emotive and cognitive-behavioral therapy: A systematic review and meta-analysis (David, et al, 2017)

...this study suggests that both CBT and tDCS, either individually or in combination, have a positive therapeutic impact on enhancing executive functions, theory of mind, and depressive symptoms in women with MDD.

(David, et al, 2018)
...we argue that CBT is the gold-standard psychological treatment—as the best standard we have in the field currently available—for the following reasons [see also Hofmann et al. (2)]: (1) CBT is the most researched form of psychotherapy. (2) No other form of psychotherapy has been shown to be systematically superior to CBT; if there are systematic differences between psychotherapies, they typically favor CBT. (3) Moreover, the CBT theoretical models/mechanisms of change have been the most researched and are in line with the current mainstream paradigms of human mind and behavior (e.g., information processing). At the same time, there is clearly room for further improvement, both in terms of CBT’s efficacy/effectiveness and its underlying theories/mechanisms of change. We further argue for an integrated scientific psychotherapy, with CBT serving as the foundational platform for integration.
2015
Psychotherapy, as engaged by a licensed mental health provider, is not under the direction of the FDA
2021
States and locales around the world currently have accepted licensure and authorizations for psychotherapy to be provided by a number of clinicians including counselors, marriage and family therapists, social workers, and psychologists– none of which are medical providers or are responsible for the medical aspects of prescription-based mental healthcare as offered by general medical clinicians and psychiatric specialists such as psychiatric nurse practitioners or psychiatrists.
Psychotherapy is the least-invasive approach in the treatment of mental illness, theoretically, and medicines have historically been prescribed in conjunction with talk therapy.
Adding a medicine has traditionally meant an escalated level of care overseen by a physician. Psychotherapists support what it is the medicine is meant to be doing as it works in the body. Sometimes as it works there are side effects. In the case of psychedelic medicines like ketamine, these are manageable and transient for most people, who also describe the experience of the medicine with words like: loving, mystical, God, to Near Death Experience, terrifying, or shocking. These experiences are frequent and predictable in psychedelic medicines including LSD, MDMA, ayahausca, DMT, psilocybin and others.
Comparatively, here is the Black Box labeling to consider with sertraline (Zoloft) - a drug promoted to be prescribed for a number of mental health indications, on and off-label, including PTSD):
WARNING: SUICIDAL THOUGHTS AND BEHAVIORS
See full prescribing information for complete boxed warning.
•Antidepressants increased the risk of suicidal thoughts and behaviors in pediatric and young adult patients
•Closely monitor for clinical worsening and emergence of suicidal thoughts and behaviors
This is in addition to loss of sex drive, nausea, diarrhea, and the inability to come off of the drug without risking a physical and psychological withdrawal. Researchers in 2018 report "Antidepressants should be added to the list of drugs associated with tolerance, dependence and a withdrawal syndrome.”

Whether psychiatric drugs or psychedelic medicines are added to your mental health care plan, a licensed psychotherapist is meant to support you in going on to lead a life without reliance on a daily mental health treatment, an approach dominated by the psychiatry movement and pharmaceutical corporations who have been advertising directly to "consumers" since the mid 1980's. Media reports warn of unscrupulous ketamine clinics marketing directly to consumers next to banner ads for Johnson & Johnson's Spravato.


Psychotherapy supports clients through the risks and side effects of an antidepressant. Psychotherapy supports clients in the possibility of a personally-meaningful reunion with a sense of Self through the psychedelic-assisted psychotherapy process. Some therapists specialize in certain approaches, methods or medicines, and others provide general ongoing mental health therapy without the assistance of medicines. This highlights the necessity in psychedelic research to test their patented compounds against the generic versions, which are mostly readily available, and against other common, already-approved mental health treatments, of which CBT is one of the current gold standards.

Scopes of Practice vs Scopes of Competency
Licensed psychotherapists work within accepted Scopes of Practices, Standards of Care, and state-licensing board descriptions of legal and ethical practice. Ethically, there is the additional standard of competency in psychotherapy, with and without the addition of medicines that may affect the psychology of the client, and/or the efficacy of the cognitive behavioral therapeutic intervention. A therapist who may be competent in supporting SSRI + cognitive behavioral therapy may not be competent in supporting a client through the process of psychedelic-assisted psychotherapy if they themselves have never had the experience. A psychiatrist competent in Stan Grof’s form of psychoanalysis, or someone who specializes in somatic experiencing may be within their Scope of Practice, but may not have a scope of competency to provide effective cognitive behavioral therapy.
Adequate training in cognitive behavioral therapy, with supervised practice is essential. Adequate personal study, research, and practice with each medicine is recommended, if not medically or otherwise contraindicated, as well as ongoing continuing education, peer supervision, interdisciplinary collaboration, and professional development. While psychopharmacology is a subject area required for many psychotherapist graduate programs and part of ongoing continuing education requirements for counselors, training in cognitive behavioral therapy is, unfortunately, not usually required training for psychiatric healthcare providers.
On the therapeutic alliance
Ketamine's "therapeutic promise is increasingly understood to involve molecular and neurobiological processes that promote neural plasticity and cognitive flexibility. These changes may create a unique window for psychotherapeutic interventions to take deeper effect." (2025)
Preliminary evidence for the importance of therapeutic alliance in MDMA-assisted psychotherapy for posttraumatic stress disorder (Zeifman, et al, 2024):
The present results provide the first preliminary evidence for the relationship between the therapeutic alliance and treatment outcomes within MDMA-AP for PTSD. These findings highlight the important role of psychotherapy, and common psychotherapeutic factors, within MDMA-AP. Replication in studies with larger and more diverse clinical samples remain necessary.
The Therapeutic Alliance: The Fundamental Element of Psychotherapy (Stubbe, 2018) :
There is consistent evidence that the quality of the therapeutic alliance is linked to the success of psychotherapeutic treatment across a broad spectrum of types of patients, treatment modalities used, presenting problems, contexts, and measurements (1–4). Although scholars may differ in how the alliance is conceptualized, most theoretical definitions of the alliance have three themes in common: the collaborative nature of the relationship, the affective bond between patient and therapist, and the patient’s and therapist’s ability to agree on treatment goals and tasks (2, 3). The therapeutic alliance is posited to be a measure of the therapist’s and client’s mutual engagement in the work of therapy—thus representing an important component for achieving treatment success, regardless of the specific treatment modality employed (3). The statistical relationship between alliance and outcome is modest—approximately 7% of the variance and an average effect size of .26. However, this link has proven to be robust across multiple meta-analyses (1–4).

In "Interpersonal factors in internet-based cognitive behavioral therapy for depression: Attachment style and alliance with the program and with the therapist” (Zalaznik, et al, 2024), researchers studied "guided internet-based cognitive behavioural therapy (ICBT) for depression”, finding:
A culturally-adapted version of ICBT for depression showed that alliance with therapist and alliance with programme both can play an important role in its effectiveness: alliance with programme and the therapist drive adherence and dropout and alliance with therapist is related to symptom improvement. Although the focus of treatment is not interpersonal, avoidant attachment style can improve following ICBT.

"The goals of the digital clinic are to improve both access to and quality of care through the ethical integration of digital technologies into clinical workflows, evidence-based care, and shared decision making in a sustainable and scalable manner. Distinct from telepsychiatry which offers synchronous telehealth, we define digital health and clinics as using asynchronous technologies such as apps and sensors to collect comprehensive data and inform care. Digital care and digital clinics can supplement telehealth (and in person care) by bringing new data into the virtual visit and offering increased support for patients between those visits." (2020)
Cognitive behavioral therapy in psychedelic medicine and ketamine research
The MAPS-sponsored study MDMA-facilitated cognitive-behavioural conjoint therapy for posttraumatic stress disorder: an uncontrolled trial (Monson, et al, 2020), researchers write:
Our initial data indicates that MDMA delivered in combination with CBCT for PTSD appears to be safe, does not appear to be treatment-interfering, and may potentiate the treatment effects for PTSD and the larger relationship context in which it exists.
This study obviously includes a review of some literature on cognitive behavioral therapy, its use in PTSD treatment as well as couples (relational) therapy. This was not, however, the study design used for MDMA-assisted psychotherapy for PTSD included in the MAPS/Lykos application presented to the FDA in 2024's New Drug Application, nor was CBT part of the Spravato application when the FDA approved esketamine in 2019.
The VA currently has an FDA-approved Phase 3 study in progress called "MDMA-assisted Brief Cognitive Behavioral Conjoint Therapy for PTSD (MDMA-bCBCT)" with results expected at the end of 2024. This study is described as "An open label, single site study assessing the preliminary effectiveness, safety, and acceptability of an intervention consisting of MDMA-assisted bCBCT".

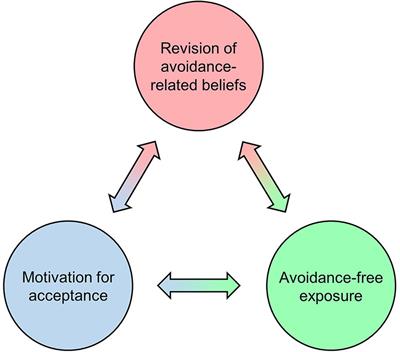
“When combined with specific context factors that are typically present in psychedelic therapy, belief relaxation can increase motivation for acceptance via operant conditioning, thus engendering episodes of relatively avoidance-free exposure to greatly intensified private events. Under these unique learning conditions, relaxed avoidance-related beliefs can be exposed to corrective experiences and become revised accordingly, potentially leading to long-term increases in acceptance and associated reductions in psychopathology. This model shows substantial parallels between psychedelic therapy and CBT that may be harnessed by using CBT as a therapeutic framework for psychedelic interventions.”

The acute subjective effects of psychedelics are responsive to users’ expectations and surroundings (i.e., “set and setting”). Accordingly, a great deal of thought has gone into designing the psychosocial context of psychedelic administration in clinical settings. But what theoretical paradigms inform these considerations about set and setting? Here, we describe several historical, sociological influences on current psychedelic administration in mainstream European and American clinical research settings, including: indigenous practices, new age spirituality from the 1960s, psychodynamic/psychoanalytic approaches, and cognitive-behavioral approaches. We consider each of these paradigms and determine that cognitive-behavioral therapies, including newer branches such as acceptance and commitment therapy (ACT), have the strongest rationale for psychedelic-assisted psychotherapy going forward. Our primary reasons for advocating for cognitive-behavioral approaches include, (1) they avoid issues of cultural insensitivity, (2) they make minimal speculative assumptions about the nature of the mind and reality, (3) they have the largest base of empirical support for their safety and effectiveness outside of psychedelic therapy. We then propose several concepts from cognitive-behavioral therapies such as CBT, DBT, and ACT that can usefully inform the preparation, session, and integration phases of psychedelic psychotherapy. Overall, while there are many sources from which psychedelic psychotherapy could draw, we argue that current gold-standard, evidence-based psychotherapeutic paradigms provide the best starting point in terms of safety and efficacy.
In McCartney, et al, 2022, "Psychedelic assisted therapy for major depressive disorder: Recent work and clinical directions”, researchers compared research into psilocybin and ketamine.
Wilkinson et al. (2017) administered ketamine in combination with cognitive behavioural therapy (CBT). Over two weeks, participants were given four ketamine infusions (0.5 mg kg−1) and concurrent, twice-weekly CBT. This psychological intervention was based on Beck's model (Disner, Beevers, Haigh, & Beck, 2011) and focused on (1) psychoeducation, (2) cognitive restructuring, and (3) behavioural modification. Immediately post-treatment, half of the participants had at least a 50% reduction in depressive symptoms. This is a roughly equivalent response rate to both Murrough et al.’s (2013)and Phillips et al. (2019) studies. In the second phase of Wilkinson et al.’s (2017) trial, they ceased ketamine administration but continued to provide 12 sessions of CBT for a further eight weeks, to determine its efficacy in prolonging ketamine's antidepressant effect. The results were supportive, showing a markedly lower relapse rate (25%) for an even longer duration (eight weeks) than the prior two studies. Furthermore, their participants took over twice as long (three months) to relapse into depression, compared to the non-CBT studies (3–5 weeks). Wilkinson et al. (2017) noted that most participants relapsed after completing weekly CBT treatment, suggesting that ongoing psychotherapy was effective in sustaining ketamine's antidepressant effect
...
This review has examined the psychedelic treatment of MDD from a multifactorial perspective. A comparison of recent clinical trials shows that the psychological component of psychedelic treatment is vital for sustaining antidepressant outcomes. This aligns with the emerging biological understanding of these substances, specifically, their capacity to induce a period of neural plasticity that enhances the opportunity for emotional, cognitive, and behavioural repatterning. Given the bias towards a medical treatment model caused by the socio-political history of psychedelics, as well as flat out ignorance of their longstanding medicinal uses in cultures across the world, future research would benefit from more deliberately considering the importance of combined psychological and psychedelic therapy. Arguably, as these substances become increasingly legalised in a medical context, and thereby accessible to the public, psychedelic therapy will become less stigmatised. Until then, acknowledgment in clinical research and by practitioners of the dual importance of biological and psychological factors, could help to present a united front that actively works to align public perception of psychedelic treatment with its true therapeutic potential.

In 2023, researchers compared the esketamine part of the ketamine molecule with and without cognitive behavioral therapy in "Cognitive behavioral therapy following esketamine for major depression and suicidal ideation for relapse prevention: The CBT-ENDURE randomized clinical trial study protocol (Kitay, et al, 2023) writing:
Cognitive behavioral therapy (CBT) effectively augments classic antidepressant medications and is highly effective in relapse prevention, especially among those with previous recurrent episodes of depression (Hollon et al., 2005; Sim et al., 2015). CBT has also been shown to prevent suicide attempts in high-risk populations over longer-term periods (Brown et al., 2005; Rudd et al., 2015). Work by our group demonstrates the feasibility and potential benefit of combining ketamine and CBT to sustain the anti-depressant effects of ketamine in severely ill, TRD patients (Wilkinson et al., 2017). A subsequent small, proof-of-concept trial showed that CBT could improve longer-term outcomes among patients treated with IV ketamine (Wilkinson et al., 2021). Here, we present the protocol for a trial that combines CBT with esketamine in patients with major depression and suicidal ideation.
...
Results of the CBT-ENDURE will have important implications for the long-term approach to patients with MDSI who receive therapy with esketamine. These study results are especially relevant for those patients who begin therapy while inpatients under the supplemental indication of esketamine, for those who live in areas remote from clinics, and for individuals for whom repeated treatments are inconvenient, uncomfortable, or cost prohibitive.
This research shows comparison to FDA-approved medicine, racemic ketamine, off label, as well as the less-effective esketamine used for its on-label indication of depression, which many forms of antidepressant drugs have not been able to treat effectively, resulting in the label treatment-resistant depression. These articles echo the evidence that cognitive behavioral therapy, with the addition of a medicine is related to positive outcomes over a longer term. In spite of this evidence, cognitive behavioral therapy is not part of the current Spravato (esketamine) plus new antidepressant as approved by the FDA in 2019.

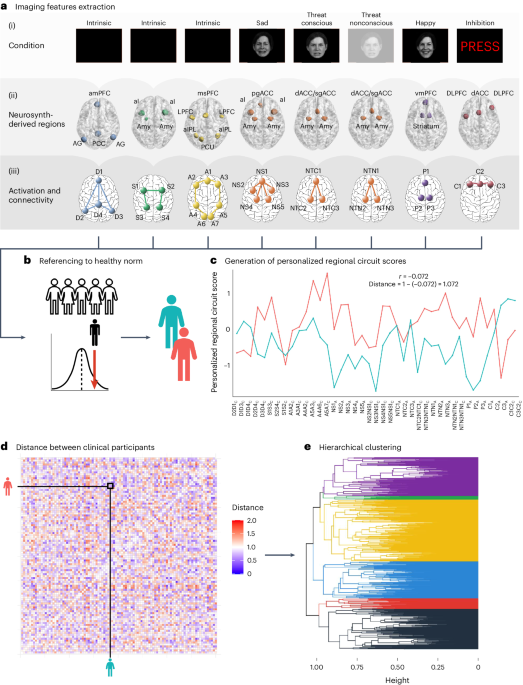
Psychedelic/ psychiatric/ neuroscience research study design should take note - there are brain scans that may indicate what type of treatment for depression and/or anxiety will work best and treatment includes cognitive behavioral therapy, also measurable in brain scans. Research directly compares 3 common antidepressants with cognitive behavioral therapy - based intervention, all reflected in brain circuit scores. The Default Mode Network (DMN) and Salience Network (SN) are well-studied in ketamine and psychedelic literature, as well as the person’s subjective experience as these brain circuits are being treated.
“Personalized brain circuit scores identify clinically distinct biotypes in depression and anxiety (Tozzi, et al, 2024):
There is an urgent need to derive quantitative measures based on coherent neurobiological dysfunctions or ‘biotypes’ to enable stratification of patients with depression and anxiety. We used task-free and task-evoked data from a standardized functional magnetic resonance imaging protocol conducted across multiple studies in patients with depression and anxiety when treatment free (n = 801) and after randomization to pharmacotherapy or behavioral therapy (n = 250). From these patients, we derived personalized and interpretable scores of brain circuit dysfunction grounded in a theoretical taxonomy. Participants were subdivided into six biotypes defined by distinct profiles of intrinsic task-free functional connectivity within the default mode, salience and frontoparietal attention circuits, and of activation and connectivity within frontal and subcortical regions elicited by emotional and cognitive tasks. The six biotypes showed consistency with our theoretical taxonomy and were distinguished by symptoms, behavioral performance on general and emotional cognitive computerized tests, and response to pharmacotherapy as well as behavioral therapy. Our results provide a new, theory-driven, clinically validated and interpretable quantitative method to parse the biological heterogeneity of depression and anxiety. Thus, they represent a promising approach to advance precision clinical care in psychiatry.
The established behavioral intervention mentioned was psychotherapy based on the underlying theories of cognitive behavioral therapy (Scott, et al, 2024). Their conclusions reflect earlier work, "New and emerging approaches to treat psychiatric disorders" (Scangos, et al, 2023) in which researchers write:
Psychiatric disorders are highly prevalent, often devastating diseases that negatively impact the lives of millions of people worldwide. Although their etiological and diagnostic heterogeneity has long challenged drug discovery, an emerging circuit-based understanding of psychiatric illness is offering an important alternative to the current reliance on trial and error, both in the development and in the clinical application of treatments. Here we review new and emerging treatment approaches, with a particular emphasis on the revolutionary potential of brain-circuit-based interventions for precision psychiatry.
Cognitive behavioral therapy, with and without psychedelic medicines including ketamine are part of these brain-circuit-based interventions. Consider this 2024 paper "Spectral signatures of psilocybin, lysergic acid diethylamide (LSD) and ketamine in healthy volunteers and persons with major depressive disorder and treatment-resistant depression: A systematic review”, (Le, et al, 2024) finding similar brain signatures for ketamine and serotonergic psychedelics (SP’s):
Ketamine and SPs are associated with increased theta power in persons with depression. Ketamine and SPs are also associated with decreased spectral power in the alpha, beta and delta bands in healthy controls and persons with depression. When administered with SPs, theta power was increased in persons with MDD when administered with SPs. Ketamine is associated with increased gamma band power in both healthy controls and persons with MDD.
...
Extant literature evaluating EEG and MEG spectral signatures indicate that ketamine and SPs have reproducible effects in keeping with disease models of network connectivity. Future research vistas should evaluate whether observed spectral signatures can guide further discovery of therapeutics within the psychedelic and dissociative classes of agents, and its prediction capability in persons treated for depression.


This is just some of the ongoing context of what has been called, “The Psychedelic Renaissance”, “The Psychedelic Hype Bubble”, and “the Wild West”. The FDA advisory committees for MDMA-Assisted Therapy, racemic ketamine and other psychedelic New Drug Applications (NDA’s) have access to this information, as do the researchers at MAPS/Lykos and the other psychedelic corporations and stakeholders in the psychedelic space. This review is ongoing.
...the greatest threat to a healthy psychedelic future is the fetishizing of just the drug alone,” adding, “Whether plant, or synthesized compound of one, there is a narrative that all you need to do to change your mind is eat something. I unknowingly contributed to that narrative.
— Rosalind Watts, psychedelic researcher, as quoted in "Some psychedelic medicine developers want to ditch the therapy aspect. What could go wrong?” (Salon, 2024).



On Esketamine sold as Spravato (2019)
Digital CBT Interventions Predict Robust Improvements in Anxiety and Depression Symptoms: A Retrospective Database Study (Holley, et al, 2024)

"The results showed significant symptom reduction across all groups, with the most pronounced effects observed in those who received concurrent psychotherapy. While infusion number did not significantly alter outcomes, the integration of ketamine with psychotherapy appeared to enhance treatment response.” (2025)
Telehealth CBT for Suicide Prevention JAMA
Part of an ongoing series and literature review of psychedelic-assisted psychotherapy, focusing on ketamine and cognitive behavioral therapy. | This information does not constitute or replace direct medical or mental health care from your providers.

The Psychedelic Institute of Mental Health & Family Therapy | Telehealth CA, NY, UT, VT | Clinical Fellowships in Psychedelic-Assisted Psychotherapy & Support | By Referral

Read more
Spotlight: Ketamine as an Adjunct Therapy for Refractory Cancer Pain: A Case Report (Emshoff, et al, 2025)"While traditionally recognized for its anesthetic and dissociative effects, low-dose, subanesthetic ketamine can be useful in palliative care to manage severe, intractable pain."By Michael DeMarco, PhDSpotlight: NPR-- Can Psychedelics Go Mainstream"Research shows that psychedelics can help with a range of mental health conditions, like PTSD and depression. "By Michael DeMarco, PhDSpotlight: "How Psychedelics Unlock Neuroplasticity for Healing""psychedelics open the brain to new patterns"By Michael DeMarco, PhDSpotlight: PBS Film-- The Last Ecstatic DaysA film about a young man with brain cancer in search of community, and the hospice doctor who gives up everything to honor his dying wish.By Michael DeMarco, PhD
- Sign up
- About
- Feed
- Founding Fellow
- INSTITUTO PSICODÉLICO DE SALUD MENTAL Y TERAPIA FAMILIAR
- Insurance + Psychedelic-Assisted Psychotherapy
- Ketamine-Assisted Psychotherapy
- Ketamine Research
- Psychedelic-Assisted Psychotherapy
- Telehealth
- Sex Therapy
- Rates, Referrals, Registration
- Practitioner DIrectory
- New York Ketamine Therapist
- Vermont Psychedelic Ketamine Therapy