About the Psychedelic Institute
Psychedelic Mental Health Community of Research, Practice & Support
Ethical psychedelic-assisted psychotherapy and psychiatric medicine-assisted psychotherapy is the collaboration between a prescribing medical care provider/s and pharmacist to monitor the medical and prescription aspects of your treatment, and mental health providers who focus on human thoughts, feelings, behaviors, and the experience of working with medicines.
The "psychedelic", "dissociative", or "psychotomimetic" experience has been suggested in research and practice around the world to be an important part of a healing process. This is done within the context of a corrective relational experience.
In other perspectives, working with a mental health practitioner can be seen as simply an intervention to minimize the side-effects of a medicine, as well as an extra layer of harm-reduction should an individual choose to work with medicine compounds that affect individual mental health.
Psychedelic practitioner specialists in pain management and mental health strive to be trusted sources for support and information as psychedelic medicines, like ketamine, become more available and more practitioners become trained in supporting psychedelic medicine experiences.
The Psychedelic Institute offers ongoing professional development and consultancy in psychedelic ketamine-assisted psychotherapy and support
You are worth getting the support you need to experience a possibility of something transformational in your life. There are medicines available that doctors may prescribe that may lead to a great reduction in human suffering. Other medicines are available in plants and fungi, which are culturally important to groups around the world spanning thousands of years. These substances are offered within contexts of authentic spiritual practice of personal, group and cultural rituals and beliefs. Psychotherapy offers a framework to make sense of the experience of being human.
A medical / mental health option
From The American Psychological Association (APA, 2024):

APA position paper on psychedelic medicines and psychotherapy
An independent medical provider trained in psychedelic medicine will make an assessment of the setting and route of administration of your ketamine treatment if they deem the off-label prescription of a medicine as beneficial in your care.

Ask your doctor for ketamine-assisted psychotherapy
See a clinician in person if you have that privilege. Telehealth increases access to a generic medicine and mental health counseling / relational therapy, which may be partially covered / reimbursed by your health insurance.
Psychedelic therapists are trained in specific medicines and modalities to prepare for the psychedelic medicine experience and to support the client beyond the acute effects of a molecule on the body
Psychedelic-assisted psychotherapy is a practice with over 100 years of research in western medicine which involves working with medicines that affect your mind, or the experience of being you- your mood, thinking, and behaviors.

(2025): "when it comes to reducing depression with psychedelic-assisted therapy, what matters even more than the drug is a strong relationship between the therapist and study participant. "
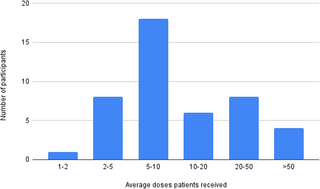
Datos clínicos del mundo real sobre la eficacia y la seguridad a largo plazo del tratamiento genérico de la ketamina racemica

(2025) "Psychedelic therapy represents a transformative shift in the treatment of mental health disorders by uniting biological mechanisms with profound psychological exploration. Through the promotion of neural plasticity, psychedelics open a window of heightened brain adaptability, creating opportunities to access and engage with core psychological processes. This unique interplay offers a powerful foundation for advancing personalized, precision-based mental health care."
Psychedelics & Cognititve Behavioral Therapy
An existential, mind-body approach
JAMA, NOV 2024
Preparation, support, and resources for ongoing integration of the various psychological and spiritual types of experiences that these medicines, practices, and states of consciousness may elicit, are all aspects of mindful, modern cognitive behavioral therapy. You may continue your mental health practice with other practitioners who come from a variety of traditions and perspectives that are culturally relevant to you and your life in the 21st Century. Cognitive behavioral therapy, known as CBT, offers a language to learn to apply in your ongoing mental health practice beyond the acute effects of the medicine. This is an intentional practice that offers a secular approach to mental health, which is evidence-based with more than 75 years of study and practice throughout the world.
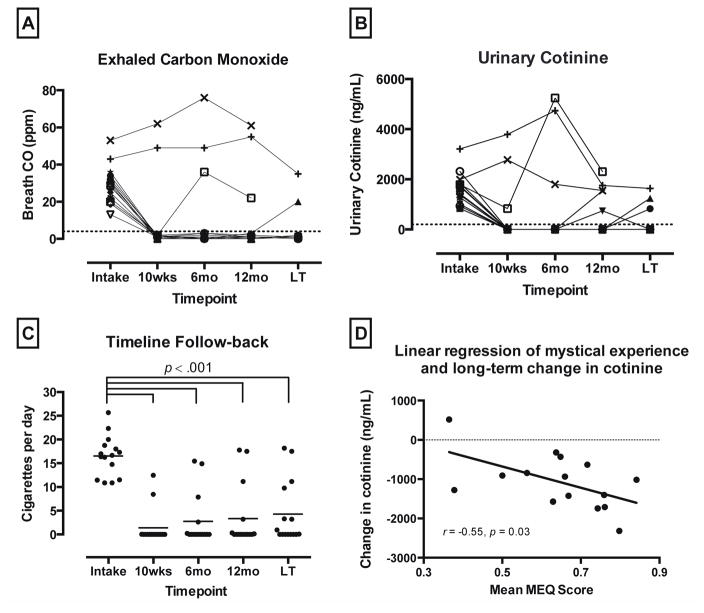
(2016): "A recent open-label pilot study (N=15) found that two to three moderate to high doses (20 and 30 mg/70 kg) of the serotonin 2A receptor agonist psilocybin, in combination with cognitive behavioral therapy (CBT) for smoking cessation, resulted in substantially higher 6-month smoking abstinence rates than are typically observed with other medications or CBT alone."

Cognitive behavioral therapy is measurable in the brain, as are the positive effects of ketamine and other molecules, especially in combination with CBT.
(2022): "...several concepts from cognitive-behavioral therapies such as CBT, DBT, and ACT can usefully inform the preparation, session, and integration phases of psychedelic psychotherapy. Overall, while there are many sources from which psychedelic psychotherapy could draw, we argue that current gold-standard, evidence-based psychotherapeutic paradigms provide the best starting point in terms of safety and efficacy."
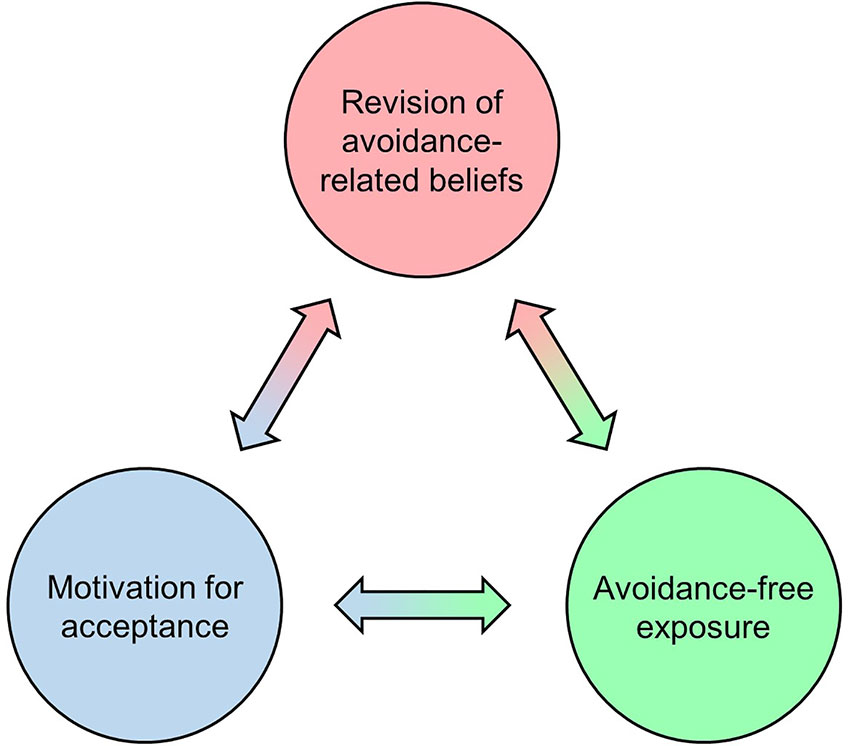
(2020): "This article presents a conceptual model that specifies potential psychological mechanisms underlying such change, and that shows substantial parallels between psychedelic therapy and cognitive behavioral therapy: We propose that in the carefully controlled context of psychedelic therapy as applied in contemporary clinical research, psychedelic-induced belief relaxation can increase motivation for acceptance via operant conditioning, thus engendering episodes of relatively avoidance-free exposure to greatly intensified private events. Under these unique learning conditions, relaxed avoidance-related beliefs can be exposed to corrective information and become revised accordingly, which may explain long-term increases in acceptance and corresponding reductions in psychopathology."
Association for Behavioral and Cognitive Therapies (ABCT): "Psychedelic-assisted therapy (PAT) is a novel form of mental health treatment that involves a combination of psychotherapy and psychedelic experiences. While PAT has been around since the 1950s, there has been a recent resurgence in clinical research and increased openness by funders, regulatory bodies, and the public to explore its potential applications."
Psychotherapy with psychedelics
Accessing and exploring various states of consciousness safely, with intention, preparation and support, followed by integrating your experiences into lasting change in your mental health and well-being, whether through meditation, psychedelic medicine, lucid dreaming, traditional plant medicine, or technodelics like vr, or binaural beats— a psychedelic experience can be the catalyst for a profound process of change. Psychotherapy is how we make sense of what happened once the medicine has left our bodies.
July 2025: Meditation and psychedelics facilitate similar types of mystical, psychological, and philosophical-existential insights predictive of wellbeing: a qualitative-quantitative approach (Jylkkä, et al, 2025)
A core value of the Institute is to approach this work in a way that is not extractive/exploitative of any particular indigenous or spiritual practice, and shows reciprocity towards any wisdom shared from people who came before the advent of our current concepts of psychology. We all come from somewhere. And we all have our individual and shared ideas as to the nature of reality, consciousness, and whether there are non-human intelligences out there in the universe in some form or another.
Invasive, colonizing groups oppress indigenous practices and beliefs as humans continue migrating around the world, as humans do. Historically, medicine experiences weren’t left for a person to figure out on their own, but within the context of corrective experiences of collective healing. A wisdom approach, whether cognitive behavioral psychotherapy, or a worldview that supports making sense of the psychedelic experience using different words, is fundamental to the process.
Studying and honoring historical cultural wisdom in the spirit of intercultural reciprocity

In the randomized, double-blind, placebo-controlled phase 2 study, investigators enrolled 73 adult participants diagnosed with moderate to severe GAD. Participants were randomly assigned to complete 2 dosing sessions with either a 25 mg dose of synthetic psilocybin or placebo, which was administered in a controlled clinical setting as part of a proprietary psychotherapeutic protocol. All participants received equal hours of psychological support and preparation, ensuring that any treatment effect could be attributed to psilocybin itself and not therapeutic bias.
Psyche- (saɪki): soul, spirit, Self, inner self, innermost self, ego, inner ego, true being, essential nature, life force, vital force, inner man, inner woman, persona, identity, personality, individuality, make-up, subconscious, mind, intellect, non-self
Delic- from δείκνῡμῐ • deíknūmi, δηλόω • (dēlóō) : to show, point out to someone, to bring to light, display, portray, represent, to make known, explain, teach, prove to show, to manifest, to make apparent or known, clear
This visionary experience has been part of our collective human experience around the world and through time, resulting from various medicine and non-medicine practices, although sometimes considered as a side effect from medicines such as ketamine.

For the past 70 years, most Western medical uses of psychedelics have centered on the way these drugs can serve as an adjunct to psychological therapy, or psychotherapy. From treating alcoholism to alleviating depression and anxiety, the general idea has been that psychedelics can amplify suggestibility, increase neuroplasticity and accelerate the clinical process of psychotherapy.
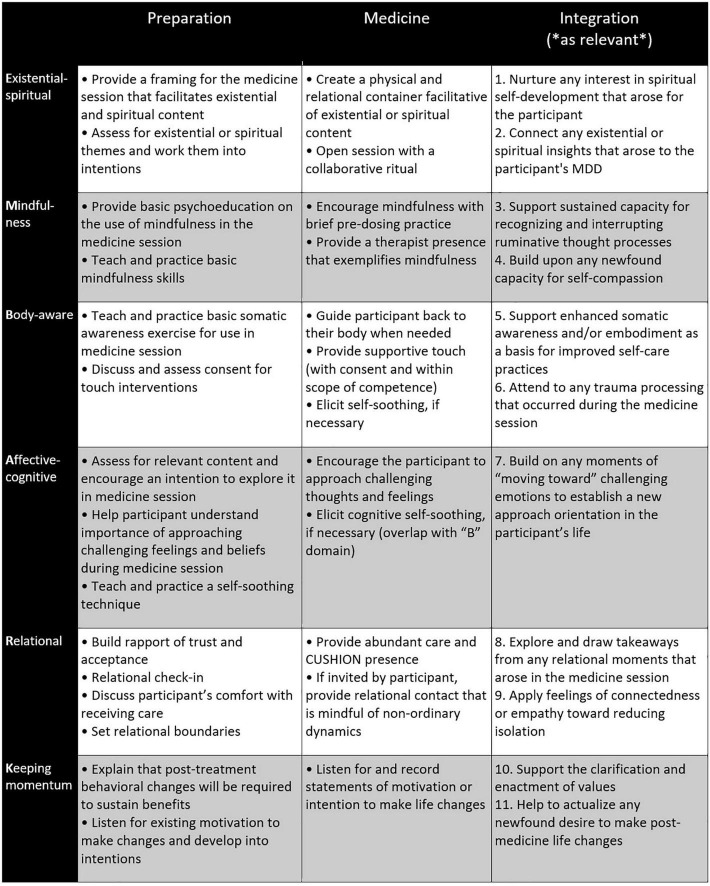
(2022): "The current standard of care in most uses of psychedelic medicines for the treatment of psychiatric indications includes the provision of a supportive therapeutic context before, during, and after drug administration. A diversity of psychedelic-assisted psychotherapy (PAP) models has been created to meet this need."
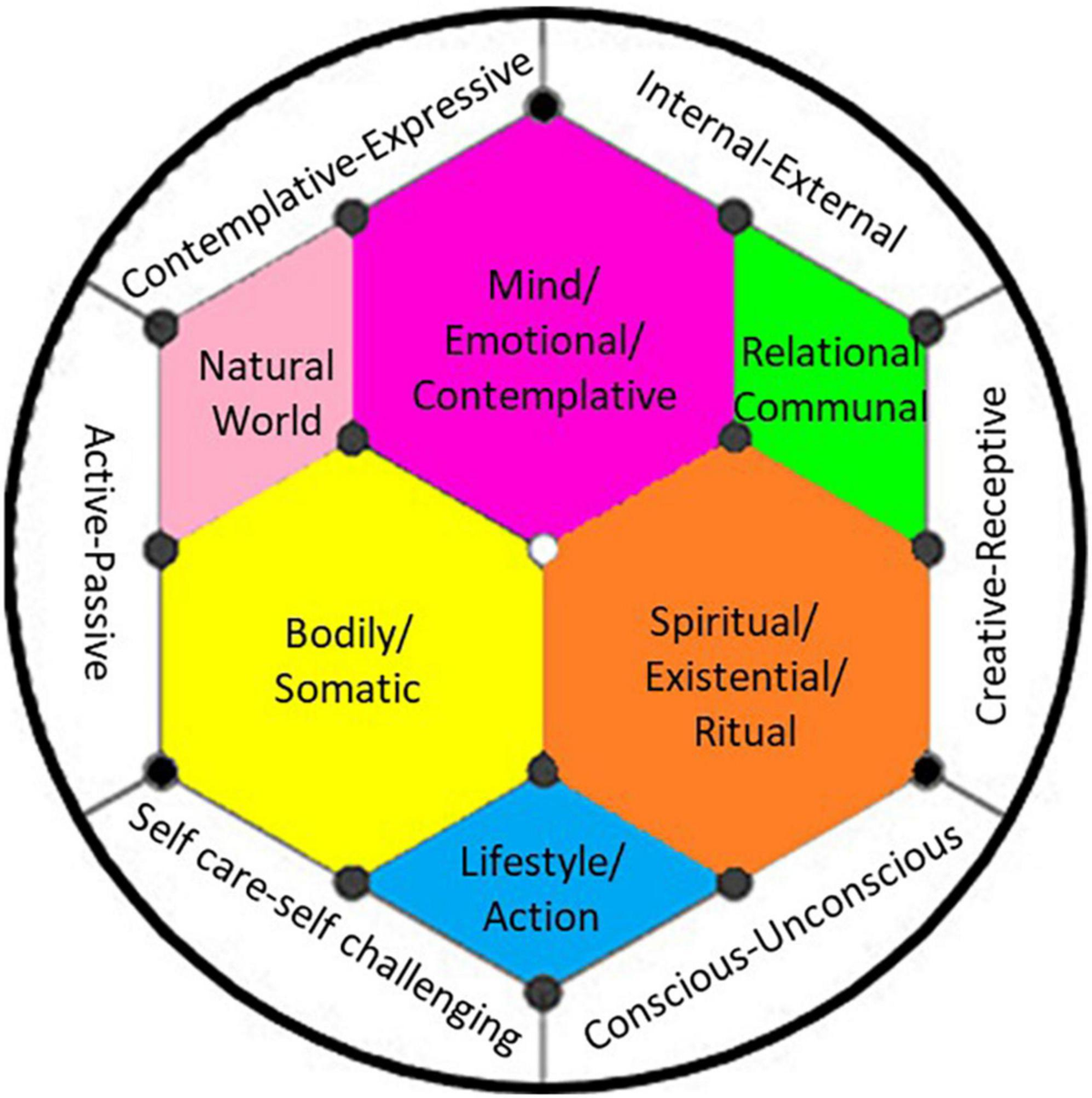
(2022) Integration is a process in which a person revisits and actively engages in making sense of, working through, translating, and processing the content of their psychedelic experience. Through intentional effort and supportive practices, this process allows one to gradually capture and incorporate the emergent lessons and insights into their lives, thus moving toward greater balance and wholeness, both internally (mind, body, and spirit) and externally (lifestyle, social relations, and the natural world).
A Community of Practice & Study
Psychedelic practicum and supervision continues after psychedelic training
As underground therapists begin to transition into above-ground practice, many are obtaining harm reduction certifications that distinguish their roles—as psychedelic facilitators or coaches—from those of licensed psychotherapists who provide psychedelic-assisted psychotherapy. Medical providers, and pharmacists oversee the clinical and pharmacological aspects of psychedelic medicine treatments.
There are responsible, collaborative ways to expand access to psychedelic care that maximize benefit while minimizing harm. One key pathway is to train licensed psychotherapists in psychedelic-assisted therapy, equipping them with the tools to guide and support this work. In turn, these trained professionals can mentor, supervise, and collaborate with non-licensed facilitators, creating a well-supported, ethical, and inclusive ecosystem of care where patients retain autonomy in their healing process, including the ability to invite trusted individuals to sit with them during their journeys or check in remotely, as is done in telehealth practice.
Together, we can build a model that prioritizes safety, accountability, and healing for the greatest number of people.
Psychedelic therapist training | Ketamine Psychedelic Practicum
The Psychedelic Institute is a community of research, practice and support, offering clinical practicums to practitioners with basic training and experience in general mental health and completion of their foundational psychedelic trainings (Certificate in Psychedelic Therapy & Research from the California Institute of Integral Studies, MAPS, Naropa, etc). The Psychedelic Institute provides clinical practicums appropriate for any level of psychedelic support and assistance, emphasizing experiential practice and clinical supervision with medical oversight and collaboration. We currently offer weekly practicums (8 hours each week) in ketamine-assisted psychotherapy & support for clinicians, chaplains, coaches, death doulas, and palliative care workers. Practice at your own pace to complete all 12 modules of Introduction and Advanced Practice in Psychedelic Ketamine Assisted Psychotherapy & Support founded on evidence-based, secular cognitive behavioral therapy, appropriate for clinicians and psychedelic practitioners.
Fall 2026 Practicum – Now Accepting Applications
Contact: https://matrix.to/#/@psychedelicmentalhealth:matrix.org
Psychedelicmentalhealth.net offers a digital manual in psychedelic cognitive behavioral therapy.
2025 Non-Clinical Fellow
Miles OHala, Smart Recovery facilitator
I’m Miles, a curious explorer at the intersection of consciousness, science, and spirituality. After years of Cognitive Behavioral Therapy and family therapy, I completed the Smart Recovery Facilitator training in January 2025 to further my own understanding of mental health techniques and group facilitation and communication skills. I devote this learning journey to understanding the transformative potential of psychedelics as tools for healing and self-discovery while also preparing to offer support to others outside of the therapy office.

2024 Clinical Fellows
Dominique Condevaux, LPC

Dominique offers ketamine-assisted psychotherapy via telehealth for clients in Michigan and Colorado. Dominique is a licensed addiction and professional counselor (National and Distance credentialed), as well as a Certified Grief Recovery Specialist with certification specialties concerning child, parent, and family issues.

I have completed 12 weeks of Ketamine practicum, and I cannot recommend this enough. What I appreciate the most is the thoughtful, insightful manner that Dr. DeMarco took when introducing the medicine to me. He shares his vast amount of information freely not only with his students but also with the Ketamine community at large. I have been sharing my experiences with my colleagues and I am asked frequently about my work with Dr. DeMarco. I feel that all psychotherapists should go through practicums such as this to experience what a client may encounter.
I feel that in addition to the previous psychedelic education, this practicum has leveled up my knowledge and experience working with Ketamine and Ketamine-Assisted Psychotherapy. Please feel free to reach out with any other questions you may have.
Dominique Condevaux LAC, LPC, MAC, ACS, BC-TMH, NCC

Thaís Salles Araujo, MD
Dr. Thaís Salles Araujo, MD is a medical doctor in California with a specialty in internal medicine and medical acupuncture. A 2023-2024 UCLA Palliative Care fellow, Thaís has experience teaching medical students, residents, and healthcare providers both in Brazil and the US. Her interests include spirituality, holistic pain care, ancient healing traditions, psychedelics, and medical education.
I’m originally from Brazil, completed internal medicine and medical acupuncture fellowship there and my personal history with the traditional use of those medicines back home is very much intertwined with my professional history in field of integrative and palliative care. I moved to the US 5 Years ago and have worked at the UCLA Center for East West medicine as a research scholar, then completed my second internal medicine residency at UCLA in the medical education pathway. My most recent projects included: assessing students perceptions and interest in the field of psychedelics and developing a curriculum for med students in integrative palliative care; co-authoring 2 book chapters in the field; psilocybin history, culture and religious aspects; Oxford University Press textbook for psychedelics for palliative care; Overview of psychedelics for palliative care, an encyclopedia of death and grief, and will present at the international conference for integrative health / academic consortium for integrative medicine in Cleveland on this topic, as well.
Dr. DeMarco is a wealth of knowledge and is so on top of the latest research and policy updates. I appreciate very much the opportunity to familiarize myself with ketamine journeys in different doses and facilitate others. It is bringing me to a more applicable deeper knowing, from this place of self experience. Feel free to reach out with any questions!

Founding Fellow 2022
Michael DeMarco, LMFT, LMHC, PhD
Supporting Membership
Access to clinician content, clinical supervision, psychedelic practicum, ketamine practicum, ongoing review of the literature, clinician community peer support, non-clinical practitioner training & support
Supporting Membership
Monthly public memberships and clinician memberships support ongoing psychedelic mental health access & advocacy
Patron, non-clinical membership
Patron members receive ongoing psychedelic mental health resources and reviews of the current psychedelic mental health industry, and access to integrative support through our Digital Clinic, curated by our Clinical Fellows and Psychedelic Mental Health Consortium members.
Membership revenues help support operational costs, help prevent AI plagiarism, create a scholarship fund for psychedelic mental health professional development programs, and increases access to psychedelic mental health practitioners to more local communities through telehealth.
Institute Fellows spend their time in research and practice when not working with clients. Institute Patrons support this ongoing review, curation and analysis as the Institute develops clinical programming for professional development.

Practitioner members receive access to the Psychedelic Institute of Mental Health & Family Therapy. network. Available for practitioners, clinicians and anyone working with medicines that may affect individual and relational (social) psychology. Once you've received your basic therapist training, our practitioner community offers psychedelic internships, apprenticeships, research support, continuing education, and psychedelic peer mentoring clinician integration and medicine retreats.
Join a community sharing interest in psychedelic-assisted therapies, plant medicines, ketamine-assisted psychotherapy, preparation, integration, and ongoing professional development in cognitive behavioral, mind-body approaches in recovery and mental health.
Psychedelics assist psychotherapy: An Introductory (P)Review of the Literature
Psychedelics may catalyze rapid improvements in mental health, but they do so firmly rooted in what we already know about the efficacy of psychotherapy. – Psychiatric Times, 2024
"The results showed significant symptom reduction across all groups, with the most pronounced effects observed in those who received concurrent psychotherapy. While infusion number did not significantly alter outcomes, the integration of ketamine with psychotherapy appeared to enhance treatment response.”
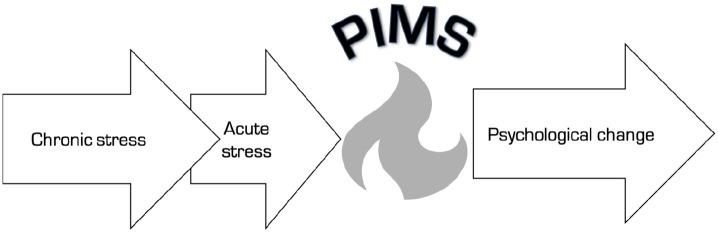
Pivotal mental states (Brouer & Carhart-Harris, 2021) This paper introduces a new construct, the ‘pivotal mental state’, which is defined as a hyper-plastic state aiding rapid and deep learning that can mediate psychological transformation. We believe this new construct bears relevance to a broad range of psychological and psychiatric phenomena. We argue that pivotal mental states serve an important evolutionary function, that is, to aid psychological transformation when actual or perceived environmental pressures demand this. We cite evidence that chronic stress and neurotic traits are primers for a pivotal mental state, whereas acute stress can be a trigger. Inspired by research with serotonin 2A receptor agonist psychedelics, we highlight how activity at this particular receptor can robustly and reliably induce pivotal mental states, but we argue that the capacity for pivotal mental states is an inherent property of the human brain itself. Moreover, we hypothesize that serotonergic psychedelics hijack a system that has evolved to mediate rapid and deep learning when its need is sensed. We cite a breadth of evidences linking stress via a variety of inducers, with an upregulated serotonin 2A receptor system (e.g. upregulated availability of and/or binding to the receptor) and acute stress with 5-HT release, which we argue can activate this primed system to induce a pivotal mental state. The pivotal mental state model is multi-level, linking a specific molecular gateway (increased serotonin 2A receptor signaling) with the inception of a hyper-plastic brain and mind state, enhanced rate of associative learning and the potential mediation of a psychological transformation.

(2024): "Psychedelics may catalyze rapid improvements in mental health, but they do so firmly rooted in what we already know about the efficacy of psychotherapy."


40 research articles were included for review: 26 studies on EBPI for PTSD, and 14 studies on PT. EBPI studied were CBT, EMDR, CPT and PE. Psychedelic compounds studied were psilocybin, ibogaine, LSD, MDMA and ketamine, for treatment of substance use disorders, anxiety relating to physical illness, depression, and PTSD. Core themes from patient experiences of EBPI: 1) patient burden in PTSD treatment; 2) readiness; 3) key mechanisms of change; 4) psychological safety and trust. Themes identified in the review of PT: 1) indirect trauma processing; 2) reorganisation of self-narratives via processes of relatedness and identification; 3) key treatment characteristics. Conclusion: This study suggests overlap between patients' experience of EBPI and PT in terms of key mechanisms of change, the importance of psychological safety and readiness to engage in treatment. Trauma-informed care paradigms and practices may improve safety and acceptability of PT research.

(Preview)

(2025): "Conventional treatments can help, but resources are limited, and suffering is profound. Ketamine-assisted psychotherapy is potentially a powerful additional resource. In the context of a trusting human relationship, it can catalyze profound exploration and relief.”
The U.S. Food and Drug Administration (FDA) approved ketamine referred to as KETARx™, on August 8th, 2025, for its indicated uses in surgical pain management.

"While risk of ketamine abuse appears low, clinicians should be alert to signs of misuse, particularly with any at-home administration. There are no reports of hypertensive emergency with ketamine treatment in the literature, or in this survey of real world use, this would be an exceedingly rare effect, not dissimilar to hypertensive crisis with monoamine oxidase inhibitors, which patients routinely use at home." (Stuart, et al, 2025)
(2025): "The overlap of MeUD with HIV risks and psychological trauma underscores the need for innovative, accessible and culturally responsive therapies. Ketamine-assisted psychotherapy (KAP), which has shown promise for treatment-resistant depression and other substance use disorders, has yet to be explored for MeUD."

(2025): "... adding combined sensory interventions to ketamine infusion enriched subjective experience. More participants in the combined sensory intervention group reported deeper engagement, a stronger sense of connection to reality, increased focus on the experience rather than the strangeness of it, moments of relief from sadness, and feelings of awe and spiritual insight compared to the control group."


(2025): "The FDA granted fast track designation to NRX-100 (NRx Pharmaceuticals, Inc), a ketamine-based drug, as a standalone therapy for the treatment of suicidal ideation in individuals with depression, including bipolar depression.1"

(2025): "With that, Norway becomes the first country to reimburse generic ketamine for treatment-resistant depression at the national level."

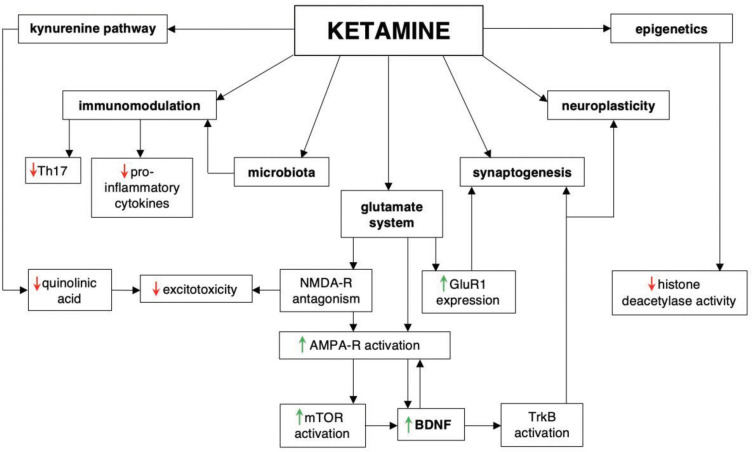
Beyond the serotonin deficit hypothesis: communicating a neuroplasticity framework of major depressive disorder (Page, et al, 2024) The serotonin deficit hypothesis explanation for major depressive disorder (MDD) has persisted among clinicians and the general public alike despite insufficient supporting evidence. To combat rising mental health crises and eroding public trust in science and medicine, researchers and clinicians must be able to communicate to patients and the public an updated framework of MDD: one that is (1) accessible to a general audience, (2) accurately integrates current evidence about the efficacy of conventional serotonergic antidepressants with broader and deeper understandings of pathophysiology and treatment, and (3) capable of accommodating new evidence. In this article, we summarize a framework for the pathophysiology and treatment of MDD that is informed by clinical and preclinical research in psychiatry and neuroscience. First, we discuss how MDD can be understood as inflexibility in cognitive and emotional brain circuits that involves a persistent negativity bias. Second, we discuss how effective treatments for MDD enhance mechanisms of neuroplasticity-including via serotonergic interventions-to restore synaptic, network, and behavioral function in ways that facilitate adaptive cognitive and emotional processing. These treatments include typical monoaminergic antidepressants, novel antidepressants like ketamine and psychedelics, and psychotherapy and neuromodulation techniques. At the end of the article, we discuss this framework from the perspective of effective science communication and provide useful language and metaphors for researchers, clinicians, and other professionals discussing MDD with a general or patient audience.

Ketamine Compared With Morphine for Out-of-Hospital Analgesia for Patients With Traumatic Pain — A Randomized Clinical Trial (Le Cornec, et al, 2024) A total of 251 patients were randomized (median age, 51 [IQR, 34-69] years; 111 women [44.9%] and 140 men [55.1%] among the 247 with data available) and were included in the intention-to-treat population. The mean pain score change was −3.7 (95% CI, −4.2 to −3.2) in the ketamine group compared with −3.8 (95% CI, −4.2 to −3.4) in the morphine group. The difference in mean pain score change was 0.1 (95% CI, −0.7 to 0.9) points. There were no clinically meaningful differences for vital signs between the 2 groups. The intravenous morphine group had 19 of 113 (16.8% [95% CI, 10.4%-25.0%]) adverse effects reported (most commonly nausea [12 of 113 (10.6%)]) compared with 49 of 120 (40.8% [95% CI, 32.0%-49.6%]) in the ketamine group (most commonly emergence phenomenon [24 of 120 (20.0%)]). No adverse events required intervention.
The MUSIK trial found that music significantly decreased ketamine-induced systolic BP changes. Music may thus represent a feasible, benign, nonpharmacological approach to improving the hemodynamic response of subanesthetic ketamine infusions for TRD. Secondary trial outcomes will be published elsewhere.
Beyond psychiatric contexts, the stimulatory hemodynamic effects of ketamine have received extensive study, both as desirable (eg, in surgical contexts) and as potentially harmful (eg, in procedural sedation),5 but never in relation to music, to our knowledge. The magnitude of the hemodynamic effects observed in this study suggests that ketamine research should consider potential influences of contextual factors, including auditory stimuli. Ketamine’s unique psychoactive effects may amplify the effects of music and other environmental influences, as has been long observed in the anesthesiology literature.

Researchers write “A sample of 11,441 patients was analyzed, At-home, telehealth-supported ketamine administration was largely safe, well-tolerated, and associated with improvement in patients with depression. Strategies for combining psychedelic-oriented therapies with rigorous telehealth models, as explored here, may uniquely address barriers to mental health treatment.”
Can Ketamine-Induced Near-Death Experiences Expedite Healing? (Sienknecht, 2020) The potential for ketamine to replicate NDE’s has been supported by research. A recent study published in Science Direct, looking at over 15,000 self-reports, found that the use of ketamine, over all other psychedelic compounds, most frequently led users to have NDE’s (followed by salvia in second and peyote in third). “After assessing the semantic similarity between 15,000 reports linked to the use of 165 psychoactive substances and 625 NDE narratives, we determined that the N-methyl-D-aspartate (NMDA) receptor antagonist ketamine consistently resulted in reports most similar to those associated with NDE’s.” The authors go on to suggest that “ketamine could be used as a safe and reversible experimental model for NDE phenomenology”1

Ketamine’s Role in Spirituality: How One Synthetic Drug Catalyzes a Natural Experience (Woods, 2020) This article highlights the potential spiritual effects of a popular anesthetic, ketamine, and how these spiritual effects can be used to help promote the reconciliation of spiritual and physical health. Ketamine, like the prominent psychedelic, psilocybin, has reportedly caused feelings of spiritual revelation and “out of body experiences” that many physicians may not feel qualified to discuss with their patients. This reluctance to address ketamine-induced spiritual experiences may affect the health outcomes of the patient. The primary goal of this project is to bring academic validity to considerations of the spiritual health of patients. This paper (1) investigates the extent that ketamine-induced, non-ordinary experiences can help bring awareness to the compatibility of spiritual and physical health and (2) compares the mechanisms of ketamine and psilocybin, as well as their value to the medical community due to the spiritual experiences that they catalyze. Thus, this research seeks to demonstrate that understanding the spiritual value of ketamine may encourage better communication between the physician and patient and promote more holistic healthcare approaches.

Cognitive neuroscience has recently become interested in altered states of consciousness such as near-death experiences (NDEs) and psychedelic experiences. While these two phenomena differ in several aspects (NDEs may occur spontaneously in life-threatening situations, while psychedelics are induced by the intake of specific substances), there are notable similarities in their phenomenology.
Within 1 h of ketamine dosing, patients reported reduced depression and anxiety ratings, which persisted for up to 7 days. A dose–response profile for ketamine was noted for dissociative side effects, adverse events and changes in blood pressure; however, changes in mood ratings were broadly similar for both ketamine doses. Overall, 14/25 patients (56%) were responders (⩾50% reduction at 24 h compared with baseline) for either ketamine dose for the Hospital Anxiety and Depression Scale (HADS), and 18/25 (72%) were responders for the HADS-anxiety scale. After fentanyl, only 1/25 (HADS-depression) and 3/25 (HADS-anxiety) were responders. Ketamine was generally safe and well tolerated in this population.
Our findings add to the literature confirming ketamine’s activity against depressive and anxiety symptoms in patients with TRD.

This scoping review describes the existing literature on the joint use of music and ketamine-or esketamine (the S(+) enantiomer of ketamine)-in humans. Exploring the Impact of Music on Response to Ketamine/Esketamine: A Scoping Review (Kheirkhah, et al, 2024)
Sublingual and iv ketamine for bipolar disorder, depression with mixed features? Ketamine in Bipolar Disorder: A Review (Wilkowska, et al, 2020) A very low dose of sublingual ketamine (administered every 2–3 days or weekly) was reported to produce rapid and consistent effects, which included the improvement of mood level and stability, cognition, and sleep in most patients (77%) with unipolar or bipolar depression; mild side effects were observed in 26 patients.21 Another study administered multiple ketamine intravenous infusions (six 0.5mg/kg infusions) in patients with unipolar (n=77) and bipolar (n=20) depression, and reported response and remission rates of 68% and 50.5%, respectively; however, the results of the bipolar group were not analyzed separately.22 A recent study on 6 low-dose ketamine infusions in 16 bipolar patients reported response and remission rate 73.7% and 63.2%, respectively, at 24 h after the 6th infusion.23 The most recent study by McIntyre included 213 TRD patients including 30 patients with bipolar disorder, but this subgroup was not analyzed separately. The authors observed rapid antidepressive and antisuicidal effects.24 The authors of the mentioned studies did not observe any significant side effects. It remains unclear as to how repeated ketamine infusions may affect the severity of subsequent episodes of bipolar depression. It is possible that this treatment regimen could decrease the severity of depressive symptoms, as well as improve quality of life and daily functioning.25 A recent retrospective study on IV ketamine in unipolar and bipolar depression suggests that using ketamine to treat resistant depression has a rapid effect in reducing agitation, irritability, anxiety, and suicidal ideation. Therefore, the authors suggest that this treatment should be considered in depression with mixed features, which is particularly common in bipolar disorders (2.2 in MDD vs 14.3% in BD) and related to high suicidality.26,27

The efficacy and safety of ketamine in the treatment of super-refractory status epilepticus: a systematic review (Yan, et al, 2024) Out of 782 studies retrieved from electronic databases, 11 met the inclusion criteria. Among them, 10 studies were retrospective, and 1 study was prospective. Patient data for inclusion were sourced from the case registries of the researchers' respective hospitals. Across all included studies, the administration of ketamine significantly reduced the duration of status epilepticus and demonstrated higher safety compared to patients not receiving ketamine treatment for super-refractory status epilepticus. Additionally, early administration of ketamine correlated with improved treatment outcomes. The risk of bias across all studies was deemed low.
(2024)
Esketamine and psilocybin NNT (number to treat) suggests safety and efficacy for depression
Psychedelic Harm Reduction Research
Ongoing review of the international psychedelic research literature
Preview
In the randomized, double-blind, placebo-controlled phase 2 study, investigators enrolled 73 adult participants diagnosed with moderate to severe GAD. Participants were randomly assigned to complete 2 dosing sessions with either a 25 mg dose of synthetic psilocybin or placebo, which was administered in a controlled clinical setting as part of a proprietary psychotherapeutic protocol. All participants received equal hours of psychological support and preparation, ensuring that any treatment effect could be attributed to psilocybin itself and not therapeutic bias.
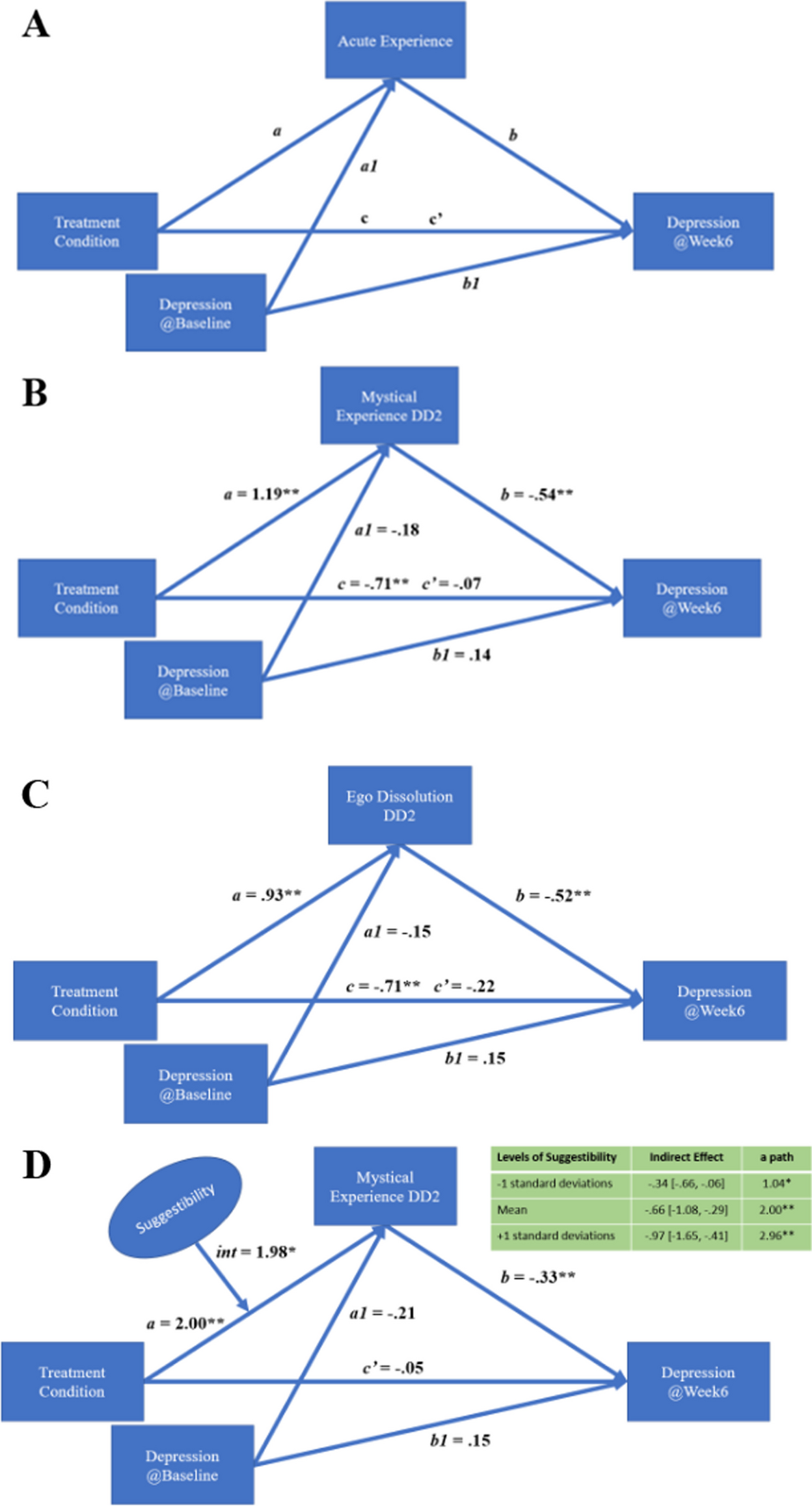
(2024) "The present study provides evidence for the role of unique psychological mechanisms underlying the therapeutic action of PT versus ET. Mystical experience and ego dissolution, in particular, demonstrated uniqueness to PT (versus ET) and meaningful associations with depressive response, while emotional breakthrough, mystical experience, and music impact were meaningfully associated with better response.Trait absorption and suggestibility showed evidence of potentiating these mechanisms, and may offer higher positive outcome prediction within a precision medicine framework. In sum, these findings advance our understanding of how psychedelic therapies may differ from conventional SSRI pharmacotherapy at the mechanistic level.These results also illustrate the value of psychological mechanisms in psychedelic therapy. Despite recent propositions about the potential sufficiency of physiological mechanisms, we remind the reader that the face valid model for psychedelic therapy involves a standard package of psychological preparation, dosing supervision with music listening and psychological integration. This is the model that has yielded the promising results that are now attracting major public and private interest in psychedelic medicine. The idea of giving a psychedelic but stripping away its psychedelic subjective effects (and perhaps stripping away psychological support also) while hoping to preserve the therapeutic response is an entirely untested model in humans."
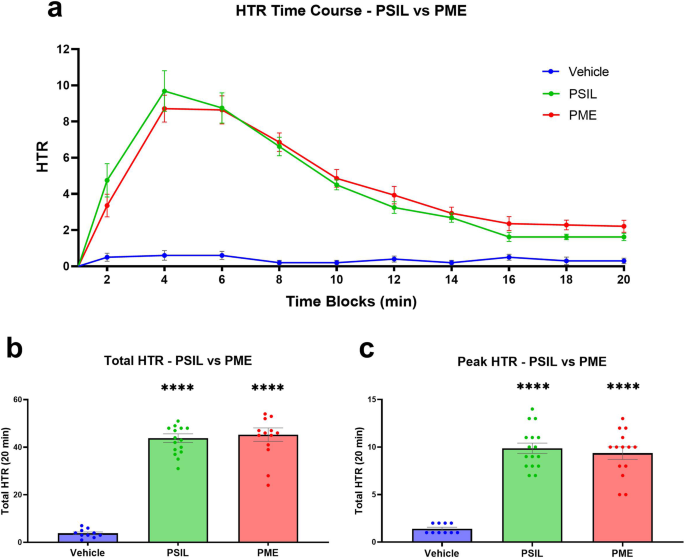
(2024): "Psilocybin, a naturally occurring, tryptamine alkaloid prodrug, is currently being investigated for the treatment of a range of psychiatric disorders. Preclinical reports suggest that the biological effects of psilocybin-containing mushroom extract or “full spectrum” (psychedelic) mushroom extract (PME), may differ from those of chemically synthesized psilocybin (PSIL)."
The present analysis suggests that psychedelic experiences, in particular those that are associated with enduring improvements in mental health, may be characterized by reproducible and predictable subtypes of the subjective psychedelic effects. These subtypes appear to be significantly different with respect to the baseline demographic characteristics, baseline measures of mental health, and drug type and dose. These findings also suggest that efforts to increase psychedelic associated personal and mystical insight experiences may be key to maximizing beneficial impact of clinical approaches using this treatment in their patients.

Direct observation of therapeutic human connection is feasible, sensitive to changes in states of consciousness and requires evaluation of audible and visual data.

Ketamine also works on glutamate. Does this make psilocybin a dissociative? Or ketamine a psychedelic? Me, myself, bye: regional alterations in glutamate and the experience of ego dissolution with psilocybin (Mason, et al, 2020)
Following a double-blind, placebo-controlled, parallel group design, we utilized an ultra-high field multimodal brain imaging approach and demonstrated that psilocybin (0.17 mg/kg) induced region-dependent alterations in glutamate, which predicted distortions in the subjective experience of one’s self (ego dissolution). Whereas higher levels of medial prefrontal cortical glutamate were associated with negatively experienced ego dissolution, lower levels in hippocampal glutamate were associated with positively experienced ego dissolution. Such findings provide further insights into the underlying neurobiological mechanisms of the psychedelic, as well as the baseline, state. Importantly, they may also provide a neurochemical basis for therapeutic effects as witnessed in ongoing clinical trials.
Psychedelic Sensationalism: An Analysis of the Schedule Classification of Psilocybin (Wood, 2023)
The importance of the social perception of different drugs in determining their eventual classification is abundantly clear. While the biochemical properties of psilocybin and other psychedelics raised few concerns, the drugs’ associations with the rebellious younger generation posed a clear threat to the American social order. Psilocybin’s importance in the hippie movement is of particular importance given the violence that hippies faced in the years leading up to the Controlled Substances Act. The persecution of hippies only intensified as a result of the Act, which supports the argument that strict enforcement of the prohibition of psilocybin had less to do with protecting the American public from the horrors of drug use and more to do with protecting the public from counterculture.
In conclusion, the lack of medical justification for the schedule classification of psilocybin alludes to a more complex explanation for its harsh criminalization. In just a matter of years, psilocybin went from being regarded as a medical marvel to being vilified as a toxic substance fit for criminals and out-of-control kids. Based on physiological data alone, psilocybin should never have been included in the Schedule I category. This calls for a more critical look at the politics surrounding drug use during the years leading up to the Controlled Substances Act. By contextualizing psilocybin’s scientific and political record within the scope of American history, it is apparent that its federal criminalization was far more complicated than a reaction to a public health concern or even a misunderstanding of its chemical effects. Psilocybin’s association with LSD and the divisive hippie movement contributed to the government’s decision to classify it as a Schedule I drug, repressing the hippies’ radical lifestyle and controversial beliefs. By implementing legal restrictions, the government could limit the spread of progressive ideology without explicitly infringing upon the freedoms of speech, expression, and protest that the hippies embraced. In an era of dramatic social change, the Controlled Substance Act bolstered traditional, conservative values and effectively criminalized American counterculture. Whether or not it was the government’s intention, the population that most threatened American traditionalism was the very demographic that was most negatively affected by psilocybin’s classification in the Controlled Substances Act. For this reason, psilocybin’s Schedule I designation in the Controlled Substances Act can be viewed as a form of social control under the thin guise of healthcare policy.
Preview
MDMA-assisted Brief Cognitive Behavioral Conjoint Therapy for ptsd (clinicaltrials.gov)
MDMA-assisted Brief Cognitive Behavioral Conjoint Therapy for ptsd (clinicaltrials.gov)
Sponsor Dr. Leslie Morland San Diego #veterans Healthcare System — #mdma research is robust and ongoing, with studies addressing the weak/sloppy areas outlined in the #fda Lykos/MAPS new drug application. #psychedelics #mdma #psychedelic #psychedelicresearch
Pure MDMA used in approved clinical settings is far safer than recreational use of Ecstasy or Molly.
•MDMA-assisted therapy could reduce social anxiety symptoms and increase social adaptability.
•The need to develop effective treatments for social anxiety in autistic adults is presently unmet.
•MDMA does not require ongoing administration to achieve lasting benefits

Big Money Is Taking Over MDMA-Assisted Therapy
Nonprofit MAPS promised to bring therapeutic MDMA to market on the back of philanthropic donations. But then it morphed into a for-profit concern — and with FDA approval looming, Big Pharma is trying to get in on the act.
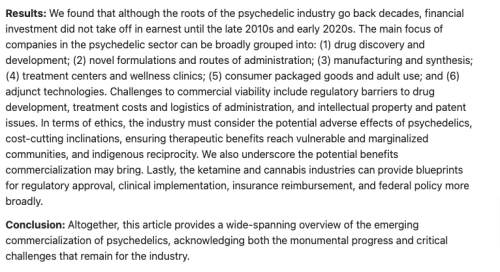
As investors pile into psychedelics, idealism gives way to pharma economics
For more than 30 years, MAPS' efforts have been funded almost entirely by donations from wealthy individuals, including billionaires like New York Mets owner Steven Cohen and Republican political donor Rebekah Mercer. On principle, MAPS has never patented its work.
The group’s pharmaceutical arm, the MAPS Public Benefit Corp., is expected to win U.S. approval this year for the first psychedelic medicine accepted for review by the Food and Drug Administration: MDMA, or ecstasy, to help treat post-traumatic stress disorder.
MDMA-Assisted Therapy Clinic Opens in AustraliaRead More →

For medical advice, please consult your State licensed healthcare provider. For psychiatric emergencies, call 988 or 911 or head to your nearest Emergency room.

Think about the media you consume and the billionaire fascists who profit.
Explore the Fediverse