Psychedelic Therapy: Does the psychedelic experience matter?
Part of an ongoing review of the literature on ketamine psychedelic-assisted psychotherapy and the phenomenology of “the psychedelic experience”
Psychedelic medicines have been studied in the Western medical literature consistently for over 100 years, over 60 of which in the ongoing study and practice of racemic ketamine in large doses as a surgical anesthetic in animals and humans, and in lower doses to treat and prevent physical and emotional pain. Psychedelic medicines, including ketamine, have consistently shown to elicit an experience, which is reflected within the brain, as measured in brain scans, which people describe as profoundly personal, and this experience, when supported by at least one other human, ideally someone trained and experienced in psychedelic-assisted psychotherapy seems to be related to an ongoing improvement in mental health.
2025
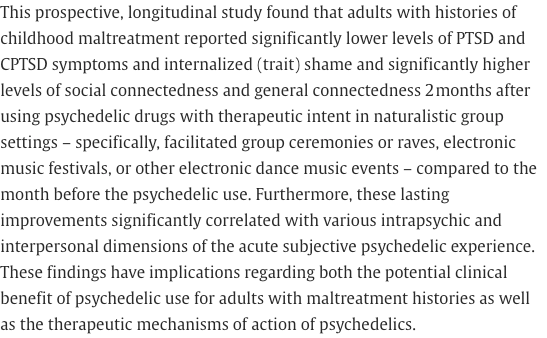
(2025): "Results revealed that a majority of the sample, 58%, ranked their psychedelic experience among the top 5 most meaningful events in their lives, while 85% among the top 10. These findings align well with previous research from other types of studies and other countries. Participants acknowledged challenging and mystical aspects as part of their psychedelic experiences, and a large majority, 94%, reported positive life improvements. Factors such as a personal growth motive and supportive social networks were associated with improved well-being."
(2025): "These findings suggest that ketamine can occasion mystical experiences in veterans with treatment-resistant depression. Future studies should further explore the mystical-type effects of ketamine as a potential contributor to its therapeutic effect in treatment-resistant depression."
"the reported insights were highly similar across the two types of reports, and only minor differences were observed between classic and non-classic psychedelics. Regression analyses indicated that metacognitive and value insights were positively associated with perceived improvements in positive affect, while mystical-type insights predicted increased meaning in life. These findings suggest that both psychedelic substances and meditation can facilitate a broad range of insights that are not fully captured by existing questionnaires. The results highlight similarities between psychedelic and meditation experiences supporting the notion that transformative experiences are not exclusive to classic psychedelics but can be facilitated through various means." (2025)
"All participants agreed that their experience was not only real but described it as more vivid and authentic than everyday reality. Four participants had no explanation for their experience, while one interpreted it in physiological terms. The remaining five explained their experiences using terms like “other planes or dimensions” and “universal consciousness,” aligning with some authors who use concepts such as “non-local” or “expanded consciousness” to address OBEs."

Ketamine-Occasioned Mystical Experience in Veterans with Treatment-Resistant Depression: A Retrospective Exploratory Analysis (Bhatt, et al, 2025) https://www.liebertpub.com/doi/abs/10.1089/psymed.2024.0040?journalCode=psymed

"Those who experienced emotionally intense or mystical states during ketamine sessions showed the most improvement, suggesting these effects may be key to healing. The study introduces the “Montreal Model,” a patient-centered approach blending psychiatry and psychedelic therapy in real-world clinical settings." (2025)
Exploring the transformative potential of out-of-body experiences: A pathway to enhanced empathy (Weiler, et al, 2024):


(2024): "Dissociative experiences are considered undesirable ketamine's adverse events. However, they might be crucial for ketamine's antidepressant effects, at least in some depression subtypes. Current understandings of ketamine's therapeutic potentials converge on the so-called "relaxed prior hypothesis," suggesting that glutamatergic blockage up-weights bottom-up surprising somatosensory/affective states. As a result, ketamine improves short-term plasticity in depression by enhancing sensitivity to interoceptive signals."
KETAMINE PSYCHEDELIC EXPERIENCE RELATED TO OUTCOME OF TREATMENT (PSYCHIATRIC TIMES, 2018)

(2018): "A cautious approach also seems imperative given evidence that ketamine demonstrates agonist activity at μ-opioid receptors and dopaminergic effects that may confer acute relief of depressive symptoms but also greater risk for positive drug reinforcement and dependence. With further insight into psychological responses mediated by ketamine, it may be that a therapy-based framework for ketamine administration optimizes treatment efficacy and sustainability, while also minimizing unnecessary drug exposure, adverse effects of chronic use, and dependency risk."
Ketamine therapy is a type of psychedelic-assisted psychotherapy. Studies continue to suggest a great deal of good can come from having a supported psychedelic medicine experience, especially when supported with cognitive behavioral therapy, a type of psychotherapy considered the gold standard of care, even when combined with less-effective antidepressants and/or other psychiatric drugs.
In the 2022 paper "Toward Synergies of Ketamine and Psychotherapy” (Mathai, et al, 2022) *pdf, researchers write:
“...It is valuable to recognize the similarities between ketamine and classic (serotonergic) psychedelics such as psilocybin and lysergic acid diethylamide (LSD), which produce overlapping subjective phenomena in spite of diverging pharmacological mechanisms of action (Bowdle et al., 1998; Studerus et al., 2010). For classic psychedelics, it is well-established that a subset of psychoactive effects, often referred to as mystical-type effects and characterized by a sense of unity, predict greater therapeutic response across a variety of conditions such as depression, existential distress, and substance use disorders… increasing research suggests that mystical- and peak-type experiences, such as measured by the Hood Mysticism Scale (HMS) and 11D-ASC questionnaire, increase the likelihood of various therapeutic benefits (Dakwar et al., 2014, 2018; Mollaahmetoglu et al., 2021; Rothberg et al., 2021; Sumner et al., 2021)" [when working with ketamine].
Consider Wolfson, editor of "The Ketamine Papers" (2016), with Dr. Vaid, here in 2024 in their paper "Ketamine-assisted psychotherapy, psychedelic methodologies, and the impregnable value of the subjective—a new and evolving approach" :
Psychiatry is in a growth phase in which several psychedelic medicines have entered its arena with great promise. Of these, presently, ketamine is the only medicine that may be legally prescribed. We hypothesize that at subanesthetic doses, ketamine produces a unique spectrum of altered states, ranging from psychoactive to deep ego-dissolving experiences, that are intrinsic to ketamine’s therapeutic effects. When these experiences are embedded in a therapeutic relationship—a setting—that fosters an amplification of the recipient’s subjective consciousness, personal growth, inner healing, greater clarity, and better relationships may well ensue. While much of the literature on ketamine labels its dissociative effects as ‘side effects’, alteration of consciousness is a component and unavoidable ‘effect’ of its therapeutic impact. From its inception in the clinical trials of the 1960s, ketamine was recognized for producing dissociative, psychedelic effects on consciousness in subjects as they emerged from ketamine-induced anesthesia. Unanticipated and unintegrated, these experiences of ‘emergence phenomena’ were felt to be disturbing. Accordingly, such experiences have been typically labeled as dissociative side effects. However, in a conducive set and settings, these experiences have been demonstrated to be of positive use in psychiatry and psychotherapy, providing a time-out from usual states of mind to facilitate a reshaping of self-experience along with symptomatic relief. In this way, ketamine-assisted psychotherapy (KAP) offers a new potential in psychiatry and psychotherapy that is powerfully valanced toward recognizing experience, individuality, and imagination. Essential to a successful therapeutic experience and outcome with KAP is close attention to the subjective experience, its expression by the recipient and integration of the ketamine experience as a healing opportunity."
In a 2024 study, "Experiences of Awe Mediate Ketamine’s Antidepressant Effects: Findings From a Randomized Controlled Trial in Treatment-Resistant Depression (Aepfelbacher, et al, 2024) researchers find:
"Ketamine infusion strongly induced heightened feelings of awe, and these experiences consistently mediated depression outcomes over a 1- to 30-days…”
In "New Clergy Study Echoes Roland Griffith’s Early Research" (2023), the late psychedelic researcher Roland Griffiths reported that research subjects in a new study of clergy members and psilocybin considered their psychedelic experience as “among the most spiritually and personally meaningful experiences of their lifetime”, mirroring prior research. Griffiths goes on to identify three common components of these experiences including a sense of interconnectedness, that the experience is precious or sacred, and that the awareness is absolutely true or more real than everyday consciousness.
In Psychedelics, Mystical Experience, and Therapeutic Efficacy: A Systematic Review (Ko, et al, 2022), researchers report:
Certain psychedelics, notably ketamine, can induce an NDE type of experience, which shares features with mystical experience of sacredness, ineffability and general sense of transcendence. The profundity of this experience is often perceived as life-changing.
...
In the Carhart-Harris et al. study, psilocybin was considered as a potential catalyst for acute neural plasticity leading to changes in cognition. This may lead to increased personal insight and therefore, symptom reduction.”
This is echoed again in "Experiences of Awe Mediate Ketamine's Antidepressant Effects: Findings From a Randomized Controlled Trial in Treatment-Resistant Depression (Aepfelbacher, et al, 2024), with researchers writing:
"Ketamine infusion strongly induced heightened feelings of awe, and these experiences consistently mediated depression outcomes over a 1- to 30-day period, unlike general dissociative side effects. The specific awe-inspiring properties of ketamine may contribute to its antidepressant effects.”
In "Ketamine Psychedelic Psychotherapy: Focus on its Ketamine Psychedelic Psychotherapy: Focus on its Pharmacology, Phenomenology, and Clinical Applications” (Kolp, et al, 2014), researchers find:
“…one-sixth to one-tenth of the dose used for general anesthesia, ketamine can create psychedelic experiences with disconnection from surroundings, perception of floating becoming disembodied as a mind or soul, and even dying and going to a different world…loss of reality contact appears more pronounced than with other psychedelics…
These ego-dissolving, transcendental experiences can generate some resolution of the patient’s addictive illnesses, psychological problems, and personality disorders, including spontaneous healing from chronic psychosomatic illnesses. It is important to note that transcendental experiences can occur with subanesthetic and high doses of ketamine.”
Psychiatrist and researcher Karl Jannsen wrote in 1997 in "The Ketamine Model of the Near-Death Experience: A Central Role for the N-Methyl-D-Aspartate Receptor” (*pdf)
“Near-death experiences (NDEs) can be reproduced by ketamine via blockade of receptors in the brain for the neurotransmitter glutamate, the N-methyl-D-aspartate (NMDA) receptors.”
In 2024, in "Within-subject comparison of near-death and psychedelic experiences: acute and enduring effects" (Martial, et al, 2024) researchers find:
...psychedelics as a useful model for studying mystical-like effects induced by NDEs, while highlighting distinctions in sensory experiences.
Roseman, et al write in "Quality of Acute Psychedelic Experience Predicts Therapeutic Efficacy of Psilocybin for Treatment-Resistant Depression” (2018):
“… the quality of the acute psychedelic experience is a key mediator of long-term changes in mental health. Future therapeutic work with psychedelics should recognize the essential importance of quality of experience in determining treatment efficacy and consider ways of enhancing mystical-type experiences and reducing anxiety.”
In "Classic psychedelics, health behavior, and physical health”, Simonsson, et al (2022) write:
“…several measures of the acute classic psychedelic experiences show promise as predictors of long-term outcomes”
In 1966, researchers Pahnke & Richards in "Implications of LSD and Experimental Mysticism” write:
“The form of psychedelic experience here called mystical consciousness can best be described as a dimension of experience that, when expressed on paper by an experimental subject and subsequently content-analyzed, corresponds to nine interrelated categories ... Unity, Objectivity & Reality, Transcendence of Space & Time, Sense of Sacredness, Deeply Felt Positive Mood, Paradoxicality, Alleged Ineffability, Transiency, Positive Changes in Attitude/Behavior”
In "Classic Psychedelic Use and Mechanisms of Mental Health: Exploring the Mediating Roles of Spirituality and Emotion Processing on Symptoms of Anxiety, Depressed Mood, and Disordered Eating in a Community Sample” (Lafrance, et al, 2021), researchers find:
“spirituality and emotion regulation may be mechanisms through which psychedelic use relates to improved mental health variables, including anxiety, depressed mood, and disordered eating behavior.”
Twelve Step group pioneer Bill Wilson, founder of Alcoholics Anonymous, believed other recovering alcoholics could benefit from taking LSD as a way to facilitate the “spiritual experience” he believed was necessary to successful recovery. We know this from Wilson, whose intractable depression was alleviated after taking LSD; his beliefs in the power of the drug are documented in his many writings.
“I am certain that the LSD experience has helped me very much,” Wilson writes in a 1957 letter. “I find myself with a heightened color perception and an appreciation of beauty almost destroyed by my years of depression… The sensation that the partition between ‘here’ and ‘there’ has become very thin is constantly with me.” writes Macbride in "66 years ago, the founder of Alcoholics Anonymous tried LSD — and ignited a controversy still raging today (2022).
“… ketamine-assisted psychedelic therapy of alcoholic patients induces… a positive transformation of nonverbalized (mostly unconscious) self-concept and emotional attitudes to various aspects of self and other people, positive changes in life values and purposes, important insights into the meaning of life and an increase in the level of spiritual development. Most importantly, these psychological changes were shown to favor a sober lifestyle.” Kolp, et al, in 2009 "Ketamine Enhanced Psychotherapy: Preliminary Clinical Observations on Its Effectiveness in Treating Alcoholism”.
"Ketamine Psychedelic Therapy (KPT): A Review of the Results of Ten Years of Research” (Krupitsky, et al, 2011) :
Ketamine is a prescription drug used for general anesthesia. In subanesthetic doses, it induces profound psychedelic experiences and hallucinations. The subanesthetic effect of ketamine was the hypothesized therapeutic mechanism in the authors' use of ketamine-assisted psychotherapy for alcoholism. The results of a controlled clinical trial demonstrated a considerable increase in efficacy of the authors' standard alcoholism treatment when supplemented by ketamine psychedelic therapy (KPT). Total abstinence for more than one year was observed in 73 out of Ill (65.8%) alcoholic patients in the KPT group, compared to 24% (24 out of 100 patients) of the conventional treatment control group (p<0.01). The authors' studies of the underlying psychological mechanisms of KPT have indicated that ketamine-assisted psychedelic therapy of alcoholic patients induces a harmonization of the Minnesota Multiphasic Personality Inventory (MMPI) personality profile, positive transformation of nonverbalized (mostly unconscious) self-concept and emotional attitudes to various aspects of self and other people, positive changes in life values and purposes. important insights into the meaning of life and an increase in the level of spiritual development. Most importantly, these psychological changes were shown to favor a sober lifestyle. The data from biochemical investigations showed that the phannacological action of KPT affects both monoaminergic and opioidergic neurotransmitter metabolism, i.e., those neurochemical systems which are involved in the pathogenesis of alcohol dependence. The data from EEG computer-assisted analysis demonstrated that ketamine increases theta activity in cerebrocortical regions of alcoholic patients. This is evidence of the reinforcement of limbic cortex interaction during the KPT session.
“Ketamine led to significantly greater acute mystical-type effects (by HMS) relative to the active control lorazepam; ketamine 0.71mg/kg was associated with significantly higher HMS scores than was the 0.41mg/kg dose. HMS score, but not CADSS score, was found to mediate the effect of ketamine on motivation to quit cocaine 24h post-infusion.” researchers write in "Therapeutic infusions of ketamine: do the psychoactive effects matter?"(Dakwar, et al, 2014)
“Research has suggested that the experience of awe or other kinds of psychedelic experience during ketamine administration may be correlated with more potent antidepressant effects” Bennett, et al, (2022) write in "Ketamine for Bipolar Depression: Biochemical, Psychotherapeutic, and Psychedelic Approaches”.
“Ego-dissolution and connectedness were found to potentiate the therapeutic effects of psychedelic experience by promoting improvement in psychological wellbeing across several mental health conditions, particularly depression, anxiety, and substance use disorders.” researchers write in "Being no one, being One: The role of ego-dissolution and connectedness in the therapeutic effects of psychedelic experience"(Kałużna, et al, 2022).
The Rev. John Mabry, a retired pastor with the United Church of Christ, has spent his life thinking and writing about the mystical core of the Christian tradition his exploration of the psychoactive properties of ketamine:
"My ketamine experience was very spiritually affirming. My understanding of God has changed. There is this mystery behind the universe and our religious traditions are metaphors and symbols that point at that larger reality. Our religious traditions are like user interfaces on a computer. The guts of a computer are a complete mystery to me, but because I have this user interface I can get a lot of work done. This is what religions do for us. We enter into relation with mystery and create meaning. (Can Psychedelics Guide a Mystic’s Path to Mystery? (Lucid News, 2023)
Researchers found in "Subtypes of the psychedelic experience have reproducible and predictable effects on depression and anxiety symptoms (Nikolaidis, et al, 2023):
These findings also suggest that efforts to increase psychedelic associated personal and mystical insight experiences may be key to maximizing beneficial impact of clinical approaches using this treatment in their patients.
In "Explanation of near-death experiences: a systematic analysis of case reports and qualitative research” (Hashemi, et al 2023), researchers suggest:
The most frequent near-death experiences were supernatural experiences, especially the experience of leaving the body. The basis and the content of the patterns mentioned by the NDEr's are similar, and the differences are in the explanation and the interpretation of the experience. There is a common core among them such as out-of-body experiences, passing through a tunnel, heightened senses, etc. Therefore, correct knowledge of near-death experiences leads to providing helpful answers to patients.
These experiences have been described in relation to DMT. In DMT Models the Near-Death Experience (Timmerman, et al, 2018), researchers offer:
Near-death experiences (NDEs) are complex subjective experiences, which have been previously associated with the psychedelic experience and more specifically with the experience induced by the potent serotonergic, N,N-Dimethyltryptamine (DMT). Potential similarities between both subjective states have been noted previously, including the subjective feeling of transcending one’s body and entering an alternative realm, perceiving and communicating with sentient ‘entities’ and themes related to death and dying. In this within-subjects placebo-controled study we aimed to test the similarities between the DMT state and NDEs, by administering DMT and placebo to 13 healthy participants, who then completed a validated and widely used measure of NDEs. Results revealed significant increases in phenomenological features associated with the NDE, following DMT administration compared to placebo. Also, we found significant relationships between the NDE scores and DMT-induced ego-dissolution and mystical-type experiences, as well as a significant association between NDE scores and baseline trait ‘absorption’ and delusional ideation measured at baseline. Furthermore, we found a significant overlap in nearly all of the NDE phenomenological features when comparing DMT-induced NDEs with a matched group of ‘actual’ NDE experiencers. These results reveal a striking similarity between these states that warrants further investigation.
In Neurochemical models of near-death experiences: A large-scale study based on the semantic similarity of written reports (Martial, et al, 2019) analysis indicates ketamine, like DMT, may act on similar receptors to form similar brainwaves, with similar subjective experiences related to proximity to death.
“After assessing the semantic similarity between 15,000 reports linked to the use of 165 psychoactive substances with 625 NDE {Near Death Experience} narratives, we determined that the N-methyl-D-aspartate (NMDA) receptor antagonist ketamine consistently resulted in reports most similar to those associated with NDEs. Ketamine was followed by Salvia divinorum and a series of serotonergic psychedelics, including the endogenous serotonin 2A receptor agonist N,N-Dimethyltryptamine (DMT). This similarity was driven by semantic concepts related to consciousness of the self and the environment, but also by those associated with the therapeutic, ceremonial and religious aspects of drug use. Our analysis sheds light on the long-standing link between certain drugs and the experience of “dying“, suggests that ketamine could be used as a safe and reversible experimental model for NDE phenomenology, and supports the speculation that endogenous NMDA antagonists with neuroprotective properties may be released in the proximity of death.”

(2014)
All research with LSD-assisted psychotherapy in the 1950s and the 1960s came to a halt by the early 1970s. Our study, the first in more than 40 years to evaluate safety and efficacy of LSD as an adjunct to psychotherapy, was conducted in participants with anxiety after being diagnosed with a life-threatening illness. In contrast to the shortcomings of older studies, we used a controlled, randomized, and blinded study design to meet contemporary research standards. LSD was given in a psychotherapeutic context to facilitate a deep psychedelic state, allowing the participant to encounter his/her own inner realities during an emotionally intensified dream-like “journey.”
In our study, using appropriate inclusion/exclusion criteria, detailed participant preparation, and a carefully supervised experience in a supportive psychotherapeutic setting, psychological side effects were mild and limited. There were no AEs often attributed to LSD such as prolonged anxiety (“bad trip”) or lasting psychotic or perceptional disorders (flashbacks). Congruent with studies in the past (Hintzen and Passie, 2010), the few mild somatic effects of LSD such as changes in heart rate and blood pressure were of no clinical significance.
The primary outcome variable in this study was of the STAI anxiety measure. Patients with life-threatening illnesses confront an existential threat from shortened life expectancy that often causes periods of suffering, pain, and anxiety. Congruent with earlier studies (Pahnke et al., 1970), the results in the experimental dose group show a significant reduction in state anxiety, as experienced on a daily basis. Furthermore, the more stable personality-inherent feature of anxiety proneness (trait anxiety) showed a strong trend toward reduction. Trait anxiety is not expected to be altered by short-term psychotherapy (Spielberger et al., 1970), but a comparable finding was reported in recent research with psilocybin in cancer patients that reported significant reductions of trait anxiety (although without correction for multiplicity) but not state anxiety (Grob et al., 2011). Therefore, this trait change may be supported by neurobiological effects of adjunctive use of LSD, which was originally introduced for deepening and accelerating psychotherapeutic processing (Abramson, 1967) and, in some studies, was shown to alter personality traits (MacLean et al., 2011; McGlothlin et al., 1967; Savage et al., 1966).
In Patient Experiences of Psilocybin-Assisted Psychotherapy: An Interpretative Phenomenological Analysis (Belser, et al, 2017), described as "the first qualitative study of participant experiences in psilocybin-assisted psychotherapy”, researchers write:
Semistructured interviews were carried out with 13 adult participants aged 22 to 69 years (M = 50 years) with clinically elevated anxiety associated with a cancer diagnosis. Participants received a moderate dose of psilocybin and adjunctive psychotherapy with an emphasis on the process of meaning-making. Verbatim transcribed interviews were analyzed by a five-member research team using interpretative phenomenological analysis. General themes found in all or nearly all transcripts included relational embeddedness, emotional range, the role of music as conveyor of experience, meaningful visual phenomena, wisdom lessons, revised life priorities, and a desire to repeat the psilocybin experience. Typical themes found in the majority of transcripts included the following: exalted feelings of joy, bliss, and love; embodiment; ineffability; alterations to identity; a movement from feelings of separateness to interconnectedness; experiences of transient psychological distress; the appearance of loved ones as guiding spirits; and sharing the experience with loved ones posttreatment. Variant themes found in a minority of participant transcripts include lasting changes to sense of identity, synesthesia experiences, catharsis of powerful emotion, improved relationships after treatment, surrender or “letting go,” forgiveness, and a continued struggle to integrate experience. The findings support the conclusion that psilocybin-assisted psychotherapy may provide an effective treatment for psychological distress in cancer patients. Implications for theory and treatment are discussed.
With the recent FDA-advisory committee discussion on MDMA-Assisted Psychotherapy, which included accusations that the sponsoring pharmaceutical corporation was a literal therapy cult, it is important to note that these are indeed the types of words we humans use to describe psychedelic experiences. The phenomenology of this is consistent, replicable, and quantifiable, even when a therapist is blinded to a client’s personal religious or spiritual beliefs. There may be people who want to take advantage of an individual’s experiences with medicine, or harm people who are working with a medicine, which is unethical and immoral, however harm to one or even few, does not outweigh the possible benefit to billions of suffering humans and animals around the planet. Physical abuse, religious abuse, or coercion is not a part of any sort of relationship, be that a professional relationship with a study researcher, medical or mental health provider, or a spiritual relationship with a religious authority such as a priest or curandero. Abuse, unfortunately, happens in the world, and is not unique or more prevalent in licensed psychedelic therapists offering solid, evidence-based support, care, and treatment to people working with psychedelic medicines beyond currently-available generic racemic ketamine, such as MDMA, Psilocybin, and DMT.
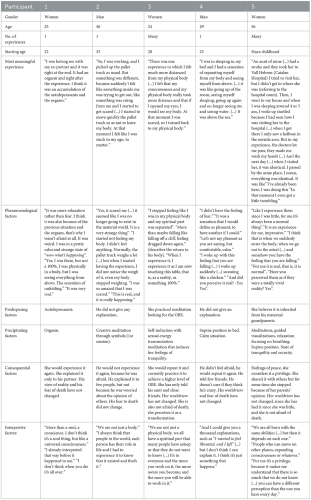
Here are clinician supervisee responses to integration questionnaires of previous participants at The Psychedelic Institute of Mental Health & Family Therapy Ketamine-Assisted Psychotherapy & Support practicum. Consider the overlapping themes found elsewhere in psychedelic research literature.
What was the most positive part of this experience?
the "knowing" of what comes after this life, the assurance. makes me want to make the most out of this one sacred life in this body.
My experience of being God. and God (me) talking to myself and comforting/reassuring me in the journey I'm on of parenting/raising a child with special needs. And seeing his future and knowing that 'he will be well. 'All will be well’
What visions or information were you able to bring home to your community about your medicine work?
All there is is LOVE - lots of love!
I think overall with the cumulative experiences, group sessions, integration calls, educational speakers and readings will benefit my work in giving ketamine to my patients and schooling that is starting soon. I've already reached out to my clinic owner and heavily encouraged her to explore possibilities of incorporating the therapy piece and integration
more relatable to my patients experiences. I'm the only staff with medicinal experiences so I feel they can find comfort in knowing they're not alone during this process.
Sharing about loving my parts of self, mothering them--that these are real part of ourselves and relationship with them matters. I was able to share my experience with both my parents and offer up a path of healing they didn't know about before.
What was the most positive part of this experience?
Learning the hard way not to waste precious sacred medicine by taking benzos
I got to meet my true higher self. I got to speak a light language back-and-forth with this other entity that is so full of love. And I have a better understanding of this light language that shows up in my journeys.
What did you feel during this experience that you would like to feel again?
Love and warmth
An overwhelming feeling of love rushing over me. Mostly a sense that everything is going to be okay, that so many of the things I worry about in the future are going to all happen when they're supposed to. That I hold all the answers.
Pure love
What was your intention before taking the medicine? How did your experience reflect your intention? How have you been incorporating this into your daily life?
Show me what was in my highest good to learn/experience. This journey was pure love. It was the mother journey
How did your experience affect your identity? Who is the person you want to become in your life and how can this experience contribute to your growth and expansion?
I saw/felt the presence of my ego during medicine session. I didn't like her. I realized that she's been feeding me lies my entire life and I've trusted her explicitly and without question. I felt anger towards her; thinking she had my best interest in mind. It was very humbling to realize that I exist outside of my ego.
What were you able to remember, carry forward, and/or complete that you had intended in your treatment?
Reconnecting with myself. Realizing that I'm so disconnected from who I am. I'm very conscious of it now.
That everything/everyone/all is somehow connected; we all come from the same source- repeating theme with treatments.
That self-love & self acceptance is the whole game. We need to mother ourselves. That is the whole goal & point of this lifetime.
What was the most negative or difficult part of your experience?
I came to the surface and thought it was over and then was surprised when I suddenly went in deeper than before and did some energy purge/release. It reminded me of my aya experience which caused some anxiety. Thankfully someone was there to really support me.
What are your intentions in life and how did this experience contribute to your larger goals and desires?
This journey moved me significantly in the direction I have been trying to go. It is hard for me to even say this but I want to become more open to connecting with a higher power. Something that happened in this journey was I had the experience that I am not yet fully comfortable with that and that I was still loved and respected. It all seemed very respectful, attuned, and consensual. Like the spirits were perfectly ok meeting me where I am at. I feel like the state of my openness to connecting with higher powers is a manifestation or reflection of my somewhat avoidant attachment style because I see the same patterns in my approach to people. So I see the openness as an openness to love in general and opening more to letting myself be loved and seen.

2024: …”the first empirical evidence suggesting that experiencing grateful affect is associated with increased longevity among older adults. The findings will need to be replicated in future studies with more representative samples"
What's happening in the brain during a psychedelic experience?
Brain circuits and brainwave patterns suggest an emerging pattern in ketamine and serotonergic psychedelic medicines.
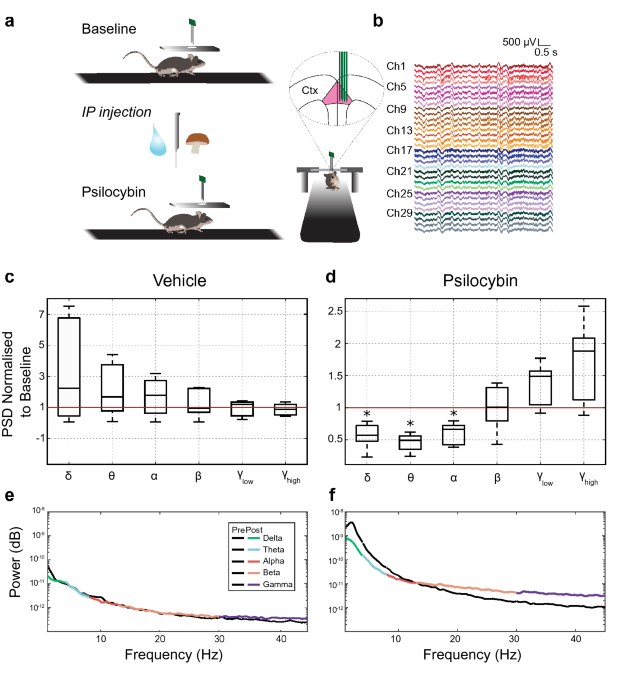
Deep posteromedial cortical rhythm in dissociation (Vesuna, et al, 2020):
Dissociation is an altered behavioural state in which the integrity of experience is disrupted, resulting in reproducible cognitive phenomena including the dissociation of stimulus detection from stimulus-related affective responses. Dissociation can occur as a result of trauma, epilepsy or dissociative drug use13,14, but despite its substantial basic and clinical importance, the underlying neurophysiology of this state is unknown. Here we establish such a dissociation-like state in mice, induced by precisely-dosed administration of ketamine or phencyclidine. Large-scale imaging of neural activity revealed that these dissociative agents elicited a 1–3-Hz rhythm in layer 5 neurons of the retrosplenial cortex.
The profound changes in perception and cognition induced by psychedelic drugs are thought to act on several levels, including increased glutamatergic activity, altered functional connectivity and an aberrant increase in high-frequency oscillations. To bridge these different levels of observation, we have here performed large-scale multi-structure recordings in freely behaving rats treated with 5-HT2AR psychedelics (LSD, DOI) and NMDAR psychedelics (ketamine, PCP). While interneurons and principal cells showed disparate firing rate modulations for the two classes of psychedelics, the local field potentials revealed a shared pattern of synchronized high-frequency oscillations in the ventral striatum and several cortical areas. Remarkably, the phase differences between structures were close to zero, corresponding to <1 ms delays. Likely, this hypersynchrony has major effects on the integration of information across neuronal systems and we propose that it is a key contributor to changes in perception and cognition during psychedelic drug use. Potentially, similar mechanisms could induce hallucinations and delusions in psychotic disorders and would constitute promising targets for new antipsychotic treatments.
In "Ketamine can produce oscillatory dynamics by engaging mechanisms dependent on the kinetics of NMDA receptors" (Adam, et al, 2024), researchers write:
Ketamine is an N-methyl-D-aspartate (NMDA)-receptor antagonist that can produce sedation, analgesia and dissociation at low doses and profound unconsciousness at high doses. It can generate gamma oscillations (>25 Hz) in the electroencephalogram which, at high-doses, are interrupted by slow-delta oscillations (0.1–4 Hz). Ketamine’s molecular targets and oscillatory dynamics have been characterized. However, how ketamine’s actions at the subcellular level give rise to the oscillatory dynamics at the network level remains unknown. Using a biophysical model of cortical circuits, we demonstrate how NMDA-receptor antagonism by ketamine produces the oscillatory dynamics recorded in humans and non-human primates. Our model analysis delivers general mechanisms that offer insight into brain dynamics, ketamine’s action on brain circuits, and ketamine’s therapeutic use for depression.
(Study models how ketamine's molecular action leads to its effects on the brain explains this further)
In a 2024 review of the literature, "Spectral signatures of psilocybin, lysergic acid diethylamide (LSD) and ketamine in healthy volunteers and persons with major depressive disorder and treatment-resistant depression: A systematic review" (Le, et al, 2024), researchers find:
Ketamine and SPs {serotonergic psychedelics} are associated with increased theta power in persons with depression. Ketamine and SPs are also associated with decreased spectral power in the alpha, beta and delta bands in healthy controls and persons with depression. When administered with SPs, theta power was increased in persons with MDD when administered with SPs. Ketamine is associated with increased gamma band power in both healthy controls and persons with MDD.
In "Characteristic patterns of EEG oscillations in sheep (Ovis aries) induced by ketamine may explain the psychotropic effects seen in humans” (Nicol & Morton, 2020) find:
"Following ketamine administration, EEG changes were immediate and widespread, affecting the full extent of the EEG frequency spectrum measured (0–125 Hz). After recovery from sedation during which low frequency activity dominated, the EEG was characterised by short periods (2–3 s) of alternating low (<14 Hz) and high (>35 Hz) frequency oscillation. This alternating EEG rhythm phase is likely to underlie the dissociative actions of ketamine, since it is during this phase that ketamine users report hallucinations. At the highest intravenous dose used (24 mg/kg), in 5/6 sheep we observed a novel effect of ketamine, namely the complete cessation of cortical EEG activity. This persisted for up to several minutes, after which cortical activity resumed. This phenomenon is likely to explain the ‘k-hole’, a state of oblivion likened to a near death experience…"
(Ketamine Experiment Reveals Brain Phenomenon Scientists Have 'Never Seen Before' explains this further)
The study of brainwaves has also recently led to the discovery of biomarkers for 6 different subtypes of anxiety and depression, which further adds to the evidence of cognitive behavioral therapy and other treatments.
Altered States of Consciousness are Prevalent and Insufficiently Supported Clinically: A Population Survey (pdf) (Wright, et al, 2024) (Writeup here) Researchers offer:
Adoption of potentially consciousness-altering practices may be leading to a rise in emergent phenomena (EP): sudden unusual mental or somatic experiences often interpreted as spiritual, mystical, energetic, or magical in nature. It is unclear how frequently these altered states of consciousness occur and what the clinical implications may be. Anecdotal accounts and prior literature suggest that EP may be common, under-reported, and followed by either positive or negative changes to well-being. We sought to supplement prior evidence on the prevalence and effects of EP among general populations with large-scale quantitative measurements.
Essentially, most experiences with different states of consciousness, even ones that arise in non-medicine practices such as meditation, are described with similar language, and felt as positive, even though the phrase “emergence phenomena” is used in the standard narrative of ketamine research as an “adverse effect” to be avoided. In this study a minority of people, 13%, felt bad after these experiences and 1% felt “life-threateningly” bad. Researchers conclude the bad experiences aren't supported enough. The study reports that 8% seek mental health help, compared to 15% seeking primary care provider help, with primary care providers being trained in treating mental illness with a daily pharmaceutical drug. Obvious question- would tying mental health counseling and psychotherapy in better with primary care help normalize the role of mental health providers in all things mindfulness and mental health care?
Exploring the transformative potential of out-of-body experiences: A pathway to enhanced empathy (Weiler, et al, 2024) write:
Out-of-body experiences (OBEs) are subjective phenomena during which individuals feel disembodied or perceive themselves as outside of their physical bodies, often resulting in profound and transformative effects. In particular, experiencers report greater heightened pro-social behavior, including more peaceful relationships, tolerance, and empathy. Drawing parallels with the phenomenon of ego dissolution induced by certain psychedelic substances, we explore the notion that OBEs may engender these changes through ego dissolution, which fosters a deep-seated sense of unity and interconnectedness with others. We then assess potential brain mechanisms underlying the link between OBEs and empathy, considering the involvement of the temporoparietal junction and the Default Mode Network. This manuscript offers an examination of the potential pathways through which OBEs catalyze empathic enhancement, shedding light on the intricate interplay between altered states of consciousness and human empathy.
The ketamine psychedelic experience, as well as the psychedelic experience linked to other medicines and non-medicine practices, is well-documented. Even when given in austere conditions, people report a good deal of positive experiences, however, the gold standard of treatment proposed here is a supported psychedelic-assisted psychotherapy process with a licensed mental health provider who specializes in cognitive behavioral therapy and its application to psychedelic medicines, particularly ketamine. This combination has precedent throughout the history of other psychiatric medicines and psychotherapy.
People have psychedelic experiences from working with certain medicines, as well as from meditation and in other altered states of consciousness. The phenomenology of this is well-studied. These experiences are often described as being profoundly beneficial when intentional, though may be frightening when unplanned.
Improving study design in psychedelic research
An ideal psychedelic trial design would compare non-medicine practices, and could be adequately blinded with ketamine, offered with and without cognitive behavioral therapy, and compared to existing psychiatric medicines. Pre-test and post-test assessments using validated mental health assessments as well as collecting quantitative (fMRI, EEG, blood samples) and qualitative (description of participant acute psychedelic experiences), and/or compared to previous research that has included these data sets. Some participants could be told in advance of the types of descriptors people use to describe psychedelic experiences, compared to another group of participants who are not pre-briefed to study consistency in psychedelic descriptions. Some participants receive cognitive behavioral therapy, others receive no support. There are ways to compare the variables and cite existing psychedelic literature in such a way to come to predictable, replicable, and generalizable conclusions. Allowing for crossover studies allows the same individual participant to describe the same experiences while participating in each group. Mixed study samples of psychedelic-naive clients compared to psychonauts with “healthy volunteers” and experienced meditators as types of control groups.
In personal and clinical practice outside of research studies, evidence does suggest that these sorts of experiences are largely beneficial for individual and social mental health. Psychedelic-assisted psychotherapy is a rational choice to support people before, sometimes during, and after a psychedelic experience.
These might be some of the finer points of #psychedelicresearch to weigh against the media sensationalism magnifying outlier cases of personal and social harm. It is important to note that the scientific study of psychedelic-assisted therapies are not the same thing as treatment. While participating in a scientific study in psychedelics may indeed be therapeutically beneficial to some participants, a clinical trial is not a replacement for ongoing mental healthcare and/or medical care.
In "Psychedelic Sensationalism: An Analysis of the Schedule Classification of Psilocybin" (Wood, 2023):
In 1970, the United States Drug Enforcement Administration passed the Controlled Substances Act. This statute classified and banned a variety of drugs including psilocybin, the psychoactive component found in Psilocybe Cubensis (also known as "Magic Mushrooms"). Though psilocybin was known to possess many medical benefits and cause no serious side effects, the Controlled Substances Act designated it as one of the most dangerous drugs, earning it a Schedule I classification. This meant possession and use incurred the highest level of legal punishment, and psilocybin could not be used under any circumstances, including in a medical setting. Based on biochemical properties alone, psilocybin does not fit the criteria to be a Schedule I drug, which suggests some other factors must have contributed to its legal classification. This paper analyzes primary and secondary sources to explore the anthropological and political motives that may have influenced psilocybin's schedule classification. The evidence that psilocybin's reputation in the eyes of the government was damaged due to its association with hippies and the counterculture movement of the 1960s and 1970s. This paper asserts that drug regulation was used as a form of social control that aimed to stifle the progressive ideals of the youth counterculture movement and reinforce conservative American ideals.
2022:
”Using multi-unit extracellular recordings, we recorded local field potential and spiking activity from populations of neurons in the anterior cingulate cortex of awake mice during the administration of psilocybin (2 mg/kg). The power of low frequency bands in the local field potential was found to significantly decrease in response to psilocybin administration, whilst gamma band activity trended towards an increase. The population firing rate was found to increase overall, with just under half of individual neurons showing a significant increase. Psilocybin significantly decreased the level of phase modulation of cells with each neural frequency band except high-gamma oscillations, consistent with a desynchronization of cortical populations. Furthermore, bursting behavior was altered in a subset of cells, with both positive and negative changes in the rate of bursting. Neurons that increased their burst firing following psilocybin administration were highly likely to transition from a phase-modulated to a phase unmodulated state. Taken together, psilocybin reduces low frequency oscillatory power, increases overall firing rates and desynchronizes local neural activity. These findings are consistent with dissolution of the default mode network under psilocybin, and may be indicative of disruption of top-down processing in the acute psychedelic state."
Part of an ongoing series. Drafts and edits ongoing (updated 6/24/24). Supporting documentation

Wolfson & Vaid, 2024

2024

(Pacheco, et al, 2024)
(Aepfelbacher, et al, 2024)
We found that the psychological experience of awe was strongly reported by participants during ketamine infusion, but not saline infusion, and there were significant associations between total AWE-S scores and Montgomery-Åsberg Depression Rating Scale score improvement (% change) in the ketamine arm at all 5 time points. Furthermore, at all 5 time points, total AWE-S scores statistically mediated the relationship between ketamine and Montgomery-Åsberg Depression Rating Scale scores. By contrast, Clinician-Administered Dissociative States Scale scores did not mediate outcomes at any time point.
Conclusions: Ketamine infusion strongly induced heightened feelings of awe, and these experiences consistently mediated depression outcomes over a 1- to 30-day period, unlike general dissociative side effects. The specific awe-inspiring properties of ketamine may contribute to its antidepressant effects.
(2025): "Furthermore, psychedelic experiences often generate encounters with what users interpret as spiritual or mystical realities [127]. These may include visions of divine beings, encounters with archetypal symbols, or feelings of profound sacredness. Such phenomena align with perennial philosophical questions about the transcendent and the numinous, experiences that evoke a sense of awe and reverence beyond ordinary understanding [128]. These mystical dimensions of psychedelics have been linked to positive therapeutic outcomes, suggesting that meaning-making processes rooted in spirituality can be integral to psychological healing,"
The Psychedelic Institute of Mental Health & Family Therapy offers clinical consultation and fellowships in psychedelic-assisted psychotherapy and support as well as individual, relational and group ketamine-assisted psychotherapy online through our connected clinicians.
#PsychedelicTherapy is #existential and processing this experience doesn't just happen safely within the walls of a psychotherapy office or posh psychedelic center. #telehealth increases access to #psychedelicassistedpsychotherapy in all 50 states #psychedelicmedicines have been studied as adjuncts to psychotherapy for over 100 years. #psychedelicresearch in #psychedelic medicines ranging from #LSD to #mdma #ketamine #dmt #ayahasuca #5meodmt #mescaline #psilocybin