Increasing Access to Psychedelic-Assisted Psychotherapy : The "proliferation of ketamine clinics" narrative and cost considerations
(ongoing edits...)
Anyone who has been written a psychiatric medication prescription by a primary care provider, their NP, PA, or a psychiatric specialist, will have noted the questions to assess for a mental health diagnosis like anxiety or depression take 5 minutes to fill out, at most. An ER visit for acute kidney stone pain where after a 9 hour wait, the attending physician prescribes an amount of opioid drugs for pain, after 37 seconds of seeing a patient... takes 9 hours and 37 seconds. Regular primary care doctor appointments in the US are billed in 15 minute increments. If a patient tells a medical provider they're anxious or depressed, meet the diagnostic criteria, and have decided the risks outweigh the benefits, they may walk out of the appointment for a medication that for some, includes the side effect is literally not being able to stop taking the daily medicine or risk withdrawal symptoms, thoughts of suicide, and risks of all types of misuse leading to harm to self or others.


How many millions of people around the world are on some form of daily psychiatric medication as a treatment for their mental health? The clinicians who follow this approach see the issue as an individual's medical problem, with a daily treatment that may improve some symptoms based on how a patient answers questions related to the diagnostic criteria invented by psychiatrists. Licensed medical clinicians practicing this way were trained this way and are practicing within their scope. It is not, however, within a physician's scope of competency (usually) to provide psychotherapy.

Psychotherapy (i.e., cognitive behavioral therapy, interpersonal therapy, behavioral activation, problem solving) may yield comparable results [4]. However, compared to pharmacotherapy, it may present a few disadvantages (patients need motivation for psychotherapy; competent psychotherapists may not be available; remission from depression tends to be slower than with pharmacotherapy) [4, 5]. Combined treatment, in particular pharmacotherapy and psychotherapy, may offer slight advantages compared to each of the treatments alone in the average case of depression. The benefits are, however, clearcut in chronic forms of mood disorders and double depression [4]. If a patient suffers from severe depression there is little doubt that pharmacotherapy may yield substantial benefits, even though, of course, response may vary from patient to patient, and meta-analyses have challenged the notion that the magnitude of benefit compared with placebo increases with severity of depression [6]. However, if symptoms of mild or moderate intensity are present, clinical trials indicate that benefits may be minimal or nonexistent [7]. Antidepressant drugs offer a number of advantages in specific clinical situations: they are readily available, they can be administered by nonpsychiatric physicians without specialized training, they act in a few weeks.
Medicine-assisted psychotherapy is supported by more than 100 years of research. In this approach, a medicine intended to have a positive effect on mental health, regardless of what that medicine is, is not presumed to fix, cure, or give life meaning simply by being ingested into the body. Working concurrently with a licensed mental health counselor or a licensed marriage and family therapist who is specially trained in medicine approaches, such as ketamine-assisted psychotherapy, supports what the medicine is doing in the brain and body, and allows for transformation and lasting change, something experienced in the mind.
While the time the therapist sits with a client on the acute effects of the medicine may or may not be covered by insurance, the preparation before taking the medicine, and the integration of the experience afterwards, can absolutely be covered by insurance using a medical structure that exists more or less around the world without the need to invent new licenses. It is important to note that in the United States, that insurance corporation will UNDERPAY the therapist, in most cases, so many psychotherapists prefer to charge a sliding scale, or offer a superbill to submit to the client's insurance plan to help with some sort of financial reimbursement directly to the client.
Decriminalizing access to medicine so that trained clinicians can support the personal decision to access this approach is essential across the range of medicines that have such effects on the human experience.
Licensed psychotherapists are some of the many types of people and professions who may support the experience of being alive on the planet which include teachers, ministers, yogi, death doulas, elder care assistants, nurses, hospice care workers, trip-sitters, life coaches, couples counselors, sex therapists, massage and physical therapists, ministers, physicians– to name but a few. Some of these specialists are licensed professionals, and others require no such license. Licensed certified professionals have a minimum standard of training and professional authority within their local communities (at the state level, for example). Any further invention of new licenses of "psychedelic facilitators" adds to the acceptance and recognition of a variety of people and pathways that may help support psychedelic practice.
Psychedelic-assisted psychotherapy is a specific modality of mental health treatment that involves the collaboration of a medical provider, and a mental health provider. In some research studies, a second trained psychedelic practitioner was required to be in the room during the acute effects of the medicine. All of these people have to have been licensed and specially trained to do this work, in addition to specially certified pharmacists.
The acute experience that may be elicited from generic compounds like MDMA or psilocybin can last for 6-8 hours. These medicines are being tweaked, then patented and brought through an FDA approval process, requiring expensive, extensive quantitative research review by competing interests.
Racemic Ketamine, also a generic compound, elicits a predictable experience lasting from 1-3 hours, and has been prescribed in various forms in various out-of-clinic settings for decades. Racemic ketamine was FDA approved as an anesthetic, found safe in high and low doses in humans and animals in 1970. Ongoing research on ketamine in humans and animals spans 60+ years.
Recently...
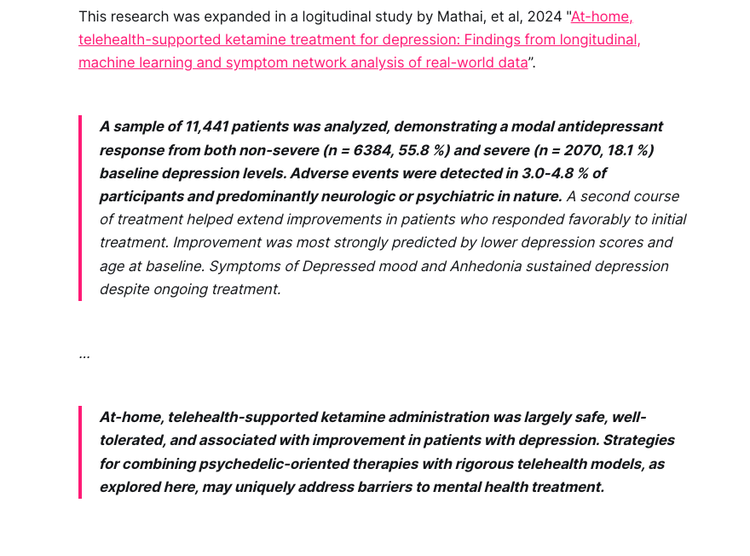

As it turns out, seeking out a psychedelic experience with no psychotherapeutic support for your click-bait article on WaPo might not be the best intentional way to approach medicines that elicit this experience
Social media click-bait headlines warn of easy access to mental health care and medicine, as if this were a bad thing, and will, no doubt, move on to other hot takes on psychedelic practice about which to panic. It is important to consider medicine given with the right support can be prescribed just as quickly and easily as prescribing medicine without that support.
Ketamine has been, and continues to be studied and prescribed off-label in conjunction with psychotherapy for treatment-resistant mood disorders ranging from anxiety to trauma. Proper screening and support requires prescribers to collaborate with certified psychedelic-assisted psychotherapy and/or psychedelic support specialists who have had documented experience with that particular medicine at the usual dosing range. "How long" it takes to get proper access to your medical provider and to some level of mental health support is a larger issue, and where the personal becomes political, requiring advocacy from each of us to demand proper medical care and mental health care to be accessible wherever needed. It's not about easy access to ketamine. It's about proper access to care, and the support needed to work towards sustained mental health.
While it may sound like media hype, when this approach is successful, clients do report profound changes that are sometimes described as mystical and lasting. Cultures around the world take various approaches to working with medicines and non-medicine approaches eliciting what has been coined psychedelic experiences. The people within each culture, who work with these medicines and practices, are fulfilling the same aforementioned roles (medical, mental health, spiritual, or other type of care provider) generally recognized and accepted within the local community. Psychotherapists and medical providers are encouraged to have first-hand experience with the medicines they prescribe when not medically / psychiatrically contraindicated to truly begin to understand what a patient may experience in the process of psychedelic-assisted psychotherapy.
On Advertising- Media reports warn of unscrupulous ketamine clinics marketing directly to consumers next to banner ads for Johnson & Johnson's Spravato, as if this were a new practice
Advertising reliance on a daily drug treatment is an approach dominated by the psychiatry movement and pharmaceutical corporations advertising directly to "consumers" since the mid 1980's.



Following the success of marketing psychiatric drugs like Prozac and Zoloft directly to vulnerable consumers, ads for Spravato by Johnson & Johnson are right next to ads for Mindbloom, as well as ads clinics offering in office sessions through less accessible routes of administration (influencer-type physicians touting their iv ketamine clinics on social media).
Only certified providers may prescribe esketamine sold as Spravato, sold from certified clinics. Do the certified Spravato doctors have a vested interest in prescribing one brand-name medicine over medicine they know exists at $12 a vial in its generic, racemic form? Isn't Johnson & Johnson hiring doctors to prescribe their drug for which they sponsored the studies? It's a problematic system that extends beyond whether there is a new IV-ketamine clinician practicing or what new startup finds a tech-savvy way to provide accessible care. How is this not a pyramid scheme?
Neither Spravato clinics nor Mindbloom collaborate with mental health providers of cognitive behavioral therapy.
Whether psychiatric drugs or psychedelic medicines are added to your mental health care plan, a licensed psychotherapist is meant to support you in going on to lead a life without reliance on a daily treatment.
Over 60 years of research has shown the predictable and replicable effects of ketamine in humans, and there are proven mental health benefits that are maximized by work with mental health specialists and support. With no contraindications, and meeting the criteria to work with this medicine, we can reframe the concern for how quickly someone can be prescribed ketamine to being concerned about making this lifesaving medicine more accessible, with proper support, to as many people as possible. The standards of practice are dictated by each provider's local license as a medical provider allowing the prescription of ketamine (or other medicines that may have effects on your thoughts/feelings/behaviors). Licensed psychotherapists specialize in medicines that assist psychotherapy, ensuring both a standard for practice (by being licensed mental health providers) and competency (by specialized training with each medicine approach). This is important context when considering the next headline about the Wild West of ketamine. In working towards healing, any approach comes with risks that should be reasonably weighed, and not ignored, whether working with a synthetic medicine like Prozac or Zoloft... or ketamine, or a traditional plant medicine like ayahausca or psilocybin mushrooms.
Now let's talk about the problems of quick access and impulsive/compulsive use of acetaminophen, alcohol, nicotine, botox, testosterone, CBD, THC, Viagra, sugar...
Cost Considerations in Psychedelic-Assisted Psychotherapy
Cost is a factor in access to cutting edge mental health treatments
Psychedelic-assisted psychotherapy with mental health specialists might be with one therapist, or a second therapist during the medicine session. One or both of those people, or a third therapist, in some cases the client's own ongoing therapist, will help to integrate the medicine experience beyond the chemical activity in the body to apply it to a peron's ongoing mental health practice. How much each of the people may charge per hour depends on their training, experience and overhead in the area in which they live. Their hourly jobs, which are often as small business owners, are to help support patients in the transformation from suffering and trauma to not needing an ongoing medication and a chance of an improved quality of life.
How much should that person make? Should they work for no pay? Should they get a subsidized education (scholarships, student loan repayment, grants) for doing this work? What about healthcare? How much does that person need to earn in order to have a chance at financial health, savings, and a retirement? If they took student loans out to do this work, should those be forgiven? These are the people TREATING the vets, first responders, the abused, the hopeless, the traumatized. These are the people trying to create a container for an experience that may lead to a transformation that it’s been described with phrases like “mystical” or “near-death experience”. Without this support, these experiences are also described as adverse effects– terrifying, useless, a funny feeling, dissociation, or something like psychosis.


How to write a hack article on ketamine -- this is 9 of hundreds of examples. Ketamine may only be prescribed by licensed medical providers working within their scope of practice and competency in the highly regulated medical industry-- hardly the "wild west". Medical providers, however, are rarely competent in mental health counseling / psychotherapy, another highly-regulated profession governed by state licensing boards, who must then pursue ongoing minimal training to meet scope of competencies within their scopes of practices.
More billable visits
There are clinicians charging upwards of $250, often more, for a 15 minute appointment, sometimes scheduling 5 appointments per hour while their nurse or staff monitors $800 sniffs of eskatamine for a bad reaction. Another version of this is upwards of $500 for a 40 minute iv visit with racemic ketamine, a generic medicine, when other routes of administration are available and have been studied and prescribed outside of iv form for decades.
On that 15 minute medical appointment– that is the reality of healthcare in the United States, not something unique to "at-home ketamine" practices like Mindbloom. Once every few months someone writes a new sensationalized article about the "Wild West of ketamine" and how quick a medical visit is in order to be prescribed ketamine, as well as panic pieces on a "proliferation of ketamine clinics" advertising online.
Spravato, a patented form of the generic drug esketamine, is advertised and sold as a weekly treatment at hundreds of dollars per dose, and is prescribed in the same 15 minute medical visit time slot as Mindbloom's offering of compounded racemic ketamine, a generic medicine sold at around the same price for 6 doses. Ketamine itself costs just a few dollars per dose. That 15 minute medical visit, whether for Spravato or compounded racemic ketamine, or for a medical visit for strep throat, or your ER visit after a 9 hour wait- these appointments costs American patients sometimes hundreds of dollars per visit. Have kidney stones (for which ketamine has been studied as a pain and trauma relief in acute kidney stone pain)? After waiting in excruciating pain in your local emergency room (looking at you Eisenhower Hospital in Rancho Mirage, California), the medical provider will prescribe you with an opioid painkiller after seeing you for 37 seconds. Seriously. A NINE HOUR WAIT, then after literally 37 seconds with the attending physician, a prescription for a month's worth of Oxtycontin with the advice "Whatever you've done in the past for kidney stones... keep doing that.".
These are examples of direct to patient advertising, originated by Republicans led by Ronald Reagan in the 1980's, shown here as examples only. The current rulers of the US want to ban pharmaceutical advertisements on television, lest they advertise any helpful medicines or vaccines. /s
It turns out, in that 15 minute medical visit, it takes just as long for your medical provider to refer you to a psychotherapist as it does to write a prescription for Zoloft, Spravato, or generic ketamine with a huge markup. Many find benefit in the psycholytic dose where the psychotherapist is able to work with newfound cognitive flexibility in a therapy session, while others find that the psychedelic approach, where you talk before and after the acute medicine experience. The therapist/s may also sit with you in every medicine session, or just in the preparation and integration sessions. Some study has been done on types of psychotherapy practices that may work during a window period after taking the medicine, such as cognitive behavioral therapy. To be a psychotherapist in the US requires at least a Masters Degree in most cases. Psychotherapists at the Masters level are required to be licensed by most states as Counselors, Marriage and Family Therapists, Social Workers, Creative Arts Therapists or Nurse Practitioners.
These people are also the unmentioned stakeholders in the news coverage of psychedelic therapy costs and insurance coverage. Most insurance companies reimburse masters level therapists right around $100 an hour, but can range from 65-125 or so. A PhD for the same procedure code? A few dollars more than that. An MD for the same code? A few dollars more than that. So whatever an individual clinician’s training, debt, fancy school, housing situation, or business overhead (marketing, malpractice insurance) may be, insurance corporations declare how much they’re paying different licensed experts for their time for the same “procedure code” per hour (which is actually 45-50 minutes because it builds in ten minutes to do a note, cry, stretch, pee, etc between clients). The mean yearly income for a masters level LMFT - $ 30.44 per hour or $ 63,300 per year — https://www.bls.gov/oes/current/oes211013.htm .
Salaries recently listed on Indeed for MD level prescribing clinicians $300-400k per year.
California recently voted to pay fast food workers $20 an hour. Compare this to 4 years of university plus 2 years for post-graduate Masters degree, then another 2-3 years of clinical supervision for licensure, then specialized training at MAPS, Fluence, PRATI, Sage, CIIS at $10000 USD or so per program, then clinical supervision for THAT. Clinical supervision is paid per hour of supervision. This is what it takes for a psychedelic therapist to help patients through what may the most vulnerable and transformative experience in healing the person has ever experienced. And this clinician has a take-home pay ten dollars above a fast-food worker. Mad props to workers. Therapists are also workers. Therapists aren’t above fast-food workers. But it seems like a question of pay for skilled vs unskilled labor, especially considering what it takes to do the work and the number of people willing to do this particular line of work. Fast-food workers need to be able to access psychedelic mental health therapy as much as any one else. Psychotherapists have specialized training at the graduate level with ongoing continuing education requirements to achieve and maintain licensure, with specialty training in psychedelics beyond that base training. There is a minimum of what they have to charge per hour to be able to do this important work with the suffering.
What value are the humans called to do this work given in all of those minor policy details which are actually very important to the quality of life of the person providing mental health support. How is their work is supported. Should they make $800 an hour?! But also, should they do it for free?! The personal branding of the clinicians, or their online clout as defined by likes and subscribes, or the branding of their educational or professional background, their office location or decor– is not what makes a mental health provider more or less valuable (or effective) in this process. Whether this work happens at a retreat, in a fancy designer office, or in community mental health or via telehealth - these folks have very specialized training in order to do this work, and are simultaneously combating ongoing narratives that psychological support offered by an actual human has no added benefit, and that simply giving people drugs is a sufficient mental health strategy. How much do THOSE workers need to make? Many psychedelic practitioners learn from indigenous world heritages spanning thousand of years which are on the verge of collapse. How much do our teachers need to earn and how are these elder practitioners and world cultures supported?

Ketamine as a generic medicine from an accredited compounding pharmacy is as affordable as those pharmacies decide to sell it based on their overhead and the supply and demand of the medicine, and has not been shown to be inferior to the brand name variant of esketamine released by J & J. It seems to work even better with a supportive wisdom approach, with psychedelic-assisted psychotherapy being one approach studied by various fields studying various compounds since the late 1800’s.

Do we minimize the value of the humans doing this work by outsourcing their gifts to AI and underpaying them or removing their value by distilling it down to brain chemistry and cutting out the human aspects covered in counseling and therapy? Not the Muskovian reality many of us want to live in. AI therapist apps have reportedly led suicides and psychosis when used without an actual human therapist connection.
Updated cost-effectiveness of MDMA-assisted therapy for the treatment of posttraumatic stress disorder in the United States: Findings from a phase 3 trial (Marseille, et al, 2022)
$11357 was the cost in the study over 42 treatment hours hours (two therapist model) and at about $270 an hour or about $135 per therapist hour.
The medical visit involves a different provider, who will have to be paid for their time and craft, same as the therapists, pharmacist and manufacturer of the medicine. (Reminder- they charge in 15 minute increments at most physician practices in the US, as well as emergency rooms and urgent care clinics.)
This study found that this IS cost-effective, and comes with great societal benefit.
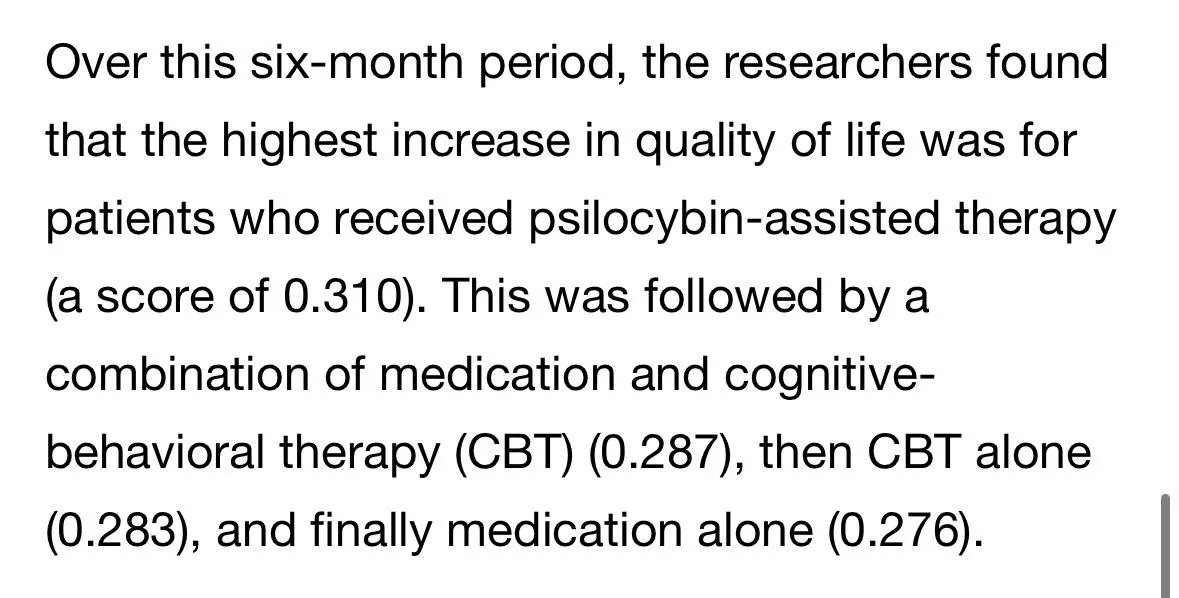
Is psychedelic-assisted psychotherapy for depression more cost-effective than conventional treatments? (2023)
The Wild West to the Rescue: Utah suggests MDMA or mushrooms should be done in medical facilities. What about Set? Setting? Support?
Utah MDMA-Assisted Therapy & Psilocybin Therapy for hospital setting only, requiring facility fees and higher cost of staffing, however using existing medical infrastructure may facilitate insurance reimbursements. (https://www.americanpatient.org/chargemaster/)
Cost involved in access to plant medicines

2025: "Psychedelic treatments in Oregon are expensive, and are likely to be so in Colorado, too, said Tasia Poinsatte, Colorado director of the nonprofit Healing Advocacy Fund, which supports state-regulated programs for psychedelic therapy. In Oregon, psychedelic mushroom sessions are typically $1,000 to $3,000, are not covered by insurance, and must be paid for up front.
The mushrooms themselves are not expensive, Poinsatte said, but a facilitator's time and support services are costly, and there are state fees. In Colorado, for doses over 2 milligrams, facilitators will screen participants at least 24 hours in advance, then supervise the session in which the participant consumes and experiences mushrooms, lasting several hours, plus a later meeting to integrate the experience.
Facilitators, who may not have experience with mental health emergencies, need training in screening, informed consent, and postsession monitoring, Smith said. "Because these models are new, we need to gather data from Colorado and Oregon to ensure safety."
Facilitators generally pay a $420 training fee, which allows them to pursue the necessary consultation hours, and roughly $900 a year for a license, and healing centers pay $3,000 to $6,000 for initial licenses in Colorado. But the up-front cost for facilitators is significant: The required 150 hours in a state-accredited program and 80 hours of hands-on training can cost $10,000 or more, and Clark said she wouldn't pursue a facilitator license due to the prohibitive time and cost.
August 2024: "What Psilocybin Costs-- It is estimated that the average journey costs about US$1,500. That includes $500-$2,000 for the facilitator, $300-$600 for the room, and $150-$200 for the psilocybin itself. For more intensive facilitation at pricier facilities, costs can be upward of $5,000 per journey."
(2025) PAT (Psilocybin-Assisted Therapy) had a 1% probability of being cost-effective when its overall costs were $10,000 and 95% when its costs were $3000. This cost-effectiveness analysis found that when its costs are $5000 or less, PAT may offer economic value compared to available TRD treatments such as Spravato (esketamine). Future studies can explore ways to reduce the cost of PAT and to understand its long-term effectiveness in maintaining remission and reducing the risk of relapse.

$4400 for 6 medicine journeys over 12 day retreat (not including airfare), in groups of 23 people at a time. That adds up to a revenue of $102120 per retreat, offered twice a month. That is about $2.5 million dollars per year of revenue. Advertising mentions "trusted by 13,000+ people". $4400 x 13000 people is over $57 million dollars.

$4500 USD for 2 medicine journeys over 5 days in Jamaica (not recommended for LGBTQ2S people due to the homophobia in this country), in groups of 15, not including airfare.
From the website Retreat Guru– "Iboga retreat pricing typically ranges from USD $550 to USD $3,000 per day, with most retreats lasting 5-9 days. Complete programs generally cost between USD $2,500 and USD $8,000 total, depending on location, program focus, and accommodations. European retreats in Spain and Portugal tend to fall in the mid-range, while ceremonies in Gabon (iboga's traditional homeland) can be more affordable at around EUR €2,300 for a 12-day initiation. Medical-focused addiction treatment programs in Mexico command premium prices, often USD $8,000-$12,000, especially for specialized protocols addressing dependencies like fentanyl."
Racemic Ketamine is currently available by prescription, is an affordable generic medicine, with years of study and administration in animals and humans from very low to very high doses. Psychotherapy treatments such as cognitive behavioral therapy have been studied for years, and are sometimes reimbursable by insurance. Affordable ketamine-assisted psychotherapy can serve as a model as other psychedelic medicines are normalized around the world as viable treatments for mental health and substance abuse disorders, especially when offered with human support.

Ketamine-assisted psychotherapy rate- $175 per hour, with programs ranging from 9 to 18 hours per program
Telehealth can be a way to increase access by keeping costs down.
This is a necessary, and ongoing conversation to have as society is deciding the value of the roles and gifts of care professionals and healers within cultures around the world. This discussion requires self-advocacy and collective bargaining, or risking being assigned a value by the billionaire venture capital investment class.
Psychedelic medicines assist psychotherapy, especially evidence-based methods such as cognitive behavioral therapy in individuals, families or groups.

The Psychedelic Institute of Mental Health & Family Therapy offers an Introductory and Advanced Ketamine-Assisted Psychotherapy training and experiential and Psychedelic Practitioner Fellowship to accomplish this interdisciplinary collaboration. This program includes 12 ketamine experiences with the medicine, as well as the opportunity to sit 12 times with someone else who has taken the medicine. Integration and support is framed with a cognitive behavioral approach. Medical clearance is required in collaboration with a medical team, overseeing assessment and prescription. Upon completion, clinicians are offered further training, practice and clinical supervision opportunities as part of our Psychedelic Practitioner Fellowship. Clinical fellows are given the opportunities to work in psychedelic preparation, support and integration and receive ongoing supervision and support from the Institute and our affiliates. Fee: $7200 USD