Ketamine Harm Reduction
Feb 2025: Ketamine Research Foundation Releases New Ketamine Guidelines for personal ketamine use
(2025):"Our findings are consistent with 2 prior reports that have highlighted the use of naltrexone in KUDs. The 2 previous case reports indicated that naltrexone at the dosage of 50 mg/day successfully helped the patients to achieve abstinence. Studies have shown that naltrexone reduces the antidepressant effects of ketamine in treatment-resistant depression, indicating an overlap between the opioid system and ketamine's NMDA receptor activity."
Ketamine, and other medicines, are often associated as the stigmatizing term "club drug". The safety and efficacy of ketamine for a number of mental health and physiological indications have been studied since 1962, however ketamine is only FDA-approved as a dissociative anesthetic and sedative. The FDA approved one half of the molecule of ketamine, esketamine, for Treatment Resistant Depression with and without suicidality. This approach supports a medical patient during the acute administration of a medicine, which must be done in specialty clinics certified by a pharmaceutical corporation, who sponsored the studies, and sell the medicine. Insurance companies may cover this approach, which also requires starting a second medicine known as an antidepressant, which is a chronic daily or several-times per week treatment for people who have been diagnosed by a physician as depressed and possibly suicidal. This requires at least 2 hours of time in the clinic, often several times a week.
(2025):"urological symptom prevalences differed little between ketamine and comparison arms. The review presented no convincing evidence of ketamine-associated uropathy arising in therapeutic contexts. The literature on ketamine-associated uropathy is critically examined; reasons for false positive uropathy findings are considered. Ketamine pharmacokinetics are described to assist the understanding of how ketamine and its metabolites may predispose to uropathy. Mechanisms of uropathy, arising from exposure to ketamine and its metabolites in urine (rather than in circulation), are summarized. A reasonable conclusion is that higher doses of ketamine, more frequent dosing with ketamine, longer duration of treatment with ketamine, and oral administration of ketamine are all potential risk factors for ketamine-associated uropathy during maintenance therapy. High hydration and frequent voiding of urine on treatment days can reduce exposure of the bladder to ketamine and its metabolites, reducing urological risks."
Ketamine prescribed off -label is a possibility for some use cases, and your medical provider and pharmacist will discuss the various indications and risks involved in various doses and routes of administration.
Talk to your independent medical provider to see if you might be a candidate for this ketamine in conjunction with cognitive behavioral therapy. Your medical provider will discuss other treatment approaches and options as indicated by ongoing, rigorous study and multidisciplinary clinical consultation. You are welcome to ask your provider for a referral for a cognitive behavioral therapy who specializes in ketamine.
The psychedelic approach in cognitive behavioral therapy emphasizes Self-discovery and reliance, working with the least amount of medicine needed for the maximum personal and social benefit and least amount of harmful side effects, referring and collaborating with your ongoing medical and mental health provider/s. Ketamine, like any psychoactive medicine prescribed for home use, has safety precautions which include setting up the ideal conditions for use.
Medicines of all types have effects on the body, positive, neutral and harmful. Working with a medical provider and mental health team offers an accessible way to a cutting-edge medicine, tending to some of the risks that come with recreational or underground use.
Ketamine is a medicine to be used in conjunction with a balanced, rational medical and mental health approach. Ketamine may elicit a personal experience with the medicine that has been described in research and anecdotally as "psychedelic".
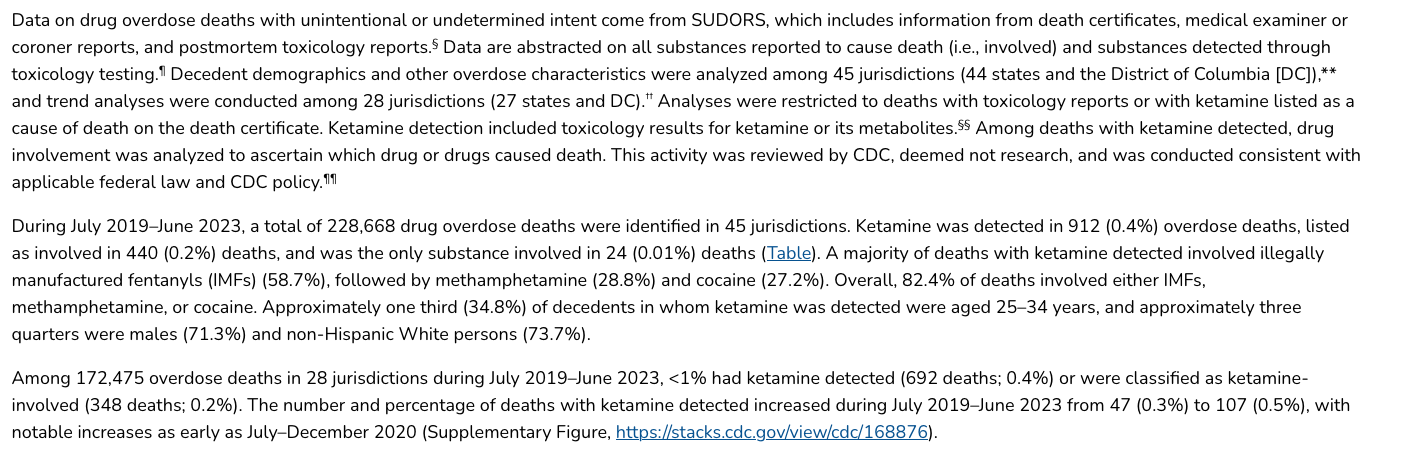
While people may come at psychedelic experiences with any sort of medicine, in any sort of location or context, ketamine in conjunction with cognitive behavioral therapy offers psycho-education to clients to prevent misuse/s of medicines which may go on to become a psychological craving in some people. There are clear cases of misuses, with deaths attributed to ketamine being occasional, yet sometimes high-profile.
Ketamine psychedelic therapy by mouth uses the minimum bio-available ketamine in a sub-anesthetic range, to maximal effect balanced between psychedelic experience and amount of medicine to elicit lasting changes in the body, in terms of pain and brain function. Cognitive behavioral therapy is a secular, evidence-based, mind-body approach to tend to what effects ketamine has on the mind and the ongoing experience of being a person in a body. For people with moderate depression, who are not in a crisis state, at-home ketamine may be an option, for others, treatment may be recommended in a psychotherapy office, psychiatry clinic, ER, or in-patient unit.
Support before, during, and after the medicine administration is essential.
If you, or someone you know is interested in ketamine harm reduction education, supervision, or support, here are some resources:





Ketamine drug interactions
On the death of Matthew Perry, the New York Times reported:
"The medical examiner’s office said that drowning, coronary artery disease and the effects of an opioid, buprenorphine, had contributed to his death. But the autopsy ascribed his death primarily to “the acute effects of ketamine.”
As noted in the above resource, 409 medications are known to interact with ketamine, including the opioid buprenorphine, noted as a possible severe interaction. Additional warnings for people with:
- heart disease;
- high blood pressure;
- liver disease;
- alcoholism; or
- if you drink large amounts of alcohol
Mixing drugs, also known as poly-drug use, or adding alcohol on top of untreated medical conditions increase risk of misuse and dangerous outcomes.
Individual reactions to ingesting something into your body, food, water, medicine, recreational drugs, alcohol, chemotherapy, antidepressants may occur, some of which are fatal. When you plan to ingest something into your body that may effect your thoughts, feelings or behaviors, consult a medical professional and a psychotherapist for counseling, especially when having feelings of harming your Self or someone else.
(2025):"There were 696 deaths identified with illicit ketamine between 1999 and 2024... the proportion of deaths where illicit ketamine was implicated in causing death declined (2014: 60.0% of cases; 2024: 42.6% of cases)." While ketamine-related deaths have been identified over the years, the proportion of cases in which illicit ketamine was the direct cause of death has significantly decreased—from 60.0% in 2014 to 42.6% in 2024—indicating progress in harm reduction efforts and possibly safer usage practices. "There has been an acceleration in deaths following illicit ketamine in recent years, which are increasingly featuring complex patterns of polydrug use and socio-economic vulnerability. Policy responses must extend beyond single-substance legislative controls to encompass harm reduction, treatment integration, and social support strategies."

Acetaminophen (Tylenol) toxicity is the second most common cause of liver transplantation worldwide and the most common cause of liver transplantation in the US. It is responsible for 56,000 emergency department visits, 2,600 hospitalizations, and 500 deaths per year in the United States. Fifty percent of these are unintentional overdoses. Perspective is important. ANY medicine may be misused.
Psychedelics in conjunction with psychotherapy is a mental health approach that has been studied and practiced in some form or another for over 100 years, and ongoing, exhaustive study of checmical compounds, including ketamine, which elicit replicable and predictable effects on people in short term use, with studies on ketamine suggesting repeated dosing in various regimens from daily to ongoing for over 18 years. There are clinical conditions that have been flagged as needing more support with this approach, requiring a medical consultation, prescription from a licensed pharmacy, and support from mental health specialists like counselors, therapists, social workers, chaplains, death doulas, hospice care worker, etc, in settings ranging from at home in bed, to group therapy sessions in retreat settings, in emergency rooms, urgent care centers, telehealth practices, and elsewhere.
If you feel in immediate danger of hurting your Self or others, please call 988 in the US, or visit https://www.iasp.info/crisis-centres-helplines/ for local assistance.

On Ketamine Bladder Risks (Mini-Review of the Literature)
Certain individuals with repeated ketamine use, especially at doses above 1 gram per day, have been reported in the literature. Consulting with your medical provider reduces the likelihood of harm to your body, and ensures ketamine remains a medicine that can help you, and not a poison that hurts you.
Multiorgan dysfunction related to chronic ketamine abuse (Pappachan, et al, 2014)
Ketamine abuse more than three times weekly for more than 2 years has been found to be a significant risk factor for urinary tract disease (9). Although recovery is observed in most cases with an early intervention, irreversible damage may occur in chronic cases.
Cholestasis related to chronic ketamine abuse has been described recently (10, 11). The exact mechanism for cholestasis is not known. Biliary dyskinesia resulting from the direct effect of the drug on the smooth muscles or through the vagus nerve may be the cause of cholestasis. Full recovery from the hepatobiliary disease over time has been observed with complete abstinence from ketamine abuse (10, 11).
Chronic abdominal pain is a common presenting complaint in ketamine abusers. The reported prevalence of upper gastrointestinal symptoms is up to 75% (2, 12). Gastritis has been demonstrated in 85% of those who had endoscopy (12). Complete relief of the symptoms is observed in most cases when patients abstain from the drug. Gastric dilatation and severe reflux esophagitis caused by chronic ketamine abuse has not been described in the medical literature previously. Ketamine has been shown to reduce the lower esophageal sphincter tone in nonhuman models (13). Smooth muscle relaxation in the upper gastrointestinal tract might have caused dysmotility, dilatation, and stasis of food in the stomach and chronic esophageal reflux in this patient. The severe cachexia mimicking malignant disease observed in our patient could have been related to upper gastrointestinal disease and the associated poor nutrition, although biliary dysfunction and acute kidney injury might have contributed to the pathogenesis.

"The results indicate that the use of single or repeated doses of esketamine at 0.25–0.5 mg/kg is unlikely to cause urothelial toxicity."
https://www.psychiatrist.com/jcp/depression/oral-ketamine-for-depression-practical-considerations/
"There were no cases of bladder toxicity."

"It should be noted that recreational ketamine consumption tends to be several orders of magnitude higher (one survey reported 34% of users reported use of 1 g or more in a typical session(Winstock et al., 2012)) than the doses prescribed in the clinical setting for depression. Although adverse effects of long-term ketamine use on the bladder would not necessarily be expected with the therapeutic dosing and frequency used in the treatment of depression, the lack of assessment of urinary symptoms has been another limitation in RCTs of ketamine (Short et al., 2018)."
https://citeseerx.ist.psu.edu/viewdoc/download?doi=10.1.1.1022.6283&rep=rep1&type=pdf
"Additionally, concerns have been raised about the possible incidence of bladder toxicity with repeated ketamine use (Middela, 2011). Only future clinical research can establish whether maintenance ketamine infusions represent a safe and effective option for initial ketamine responders."
https://www.tandfonline.com/doi/pdf/10.1080/00952990.2020.1769118
"Scientific data show that, in a clinical setting, the applied doses of ketamine are well-tolerated by humans and its negative effects are manageable. These effects seem to be dose and frequency-related, which is strongly supported by the scientific literature and by the analyzed threads, where the adverse effects of ketamine were mentioned as mild and manageable."
https://core.ac.uk/download/pdf/161939325.pdf
"The most serious of these side effects is ketamine-induced ulcerative cystitis or ‘ketamine bladder’. This is a recently identified condition characterised by extremely painful and frequent urination that seems to have severe and potentially long lasting impacts on the patient. However, drug users who take ketamine less than daily have not reported, and show no evidence of ‘ketamine bladder’.
Self Management and Recovery Training (SMART)
SMART Recovery was established in 1994 to meet the increasing demand of those seeking a secular and evidence-informed alternative to the widespread 12-Step addiction recovery program based on cognitive behavioral therapy. SMART Recovery also trains facilitators and mental health providers and allied fields.
SMART Recovery picks up with at home and community resources where cognitive behavioral therapy leaves off, especially for people dealing with problematic behaviors like substance dependence. Building this resource into the treatment plan offers another safeguard against the misuse of medicines, or other compulsive types of cravings and behaviors that end with personal and/or social harm. They offer great tools, regular meetings around the world and online.
.png)



"Emotional crisis is a universal experience. It can happen to anyone, at any time. When we are exposed to this extraordinary situation, we develop amazing and creative ways to protect ourselves, To onlookers, these protective mechanisms may look very odd, even “crazy”. To us, they have meaning. Through using eCPR we can better understand and overcome our fear of seemingly unusual behavior brought on by an emotional crisis. Through eCPR we learn how to form supportive connections that empower the person in emotional crisis so they are able to feel revitalized and quickly resume meaningful roles in the community."
National Suicide Prevention Lifeline – US: 1-800-273-TALK (8255)
http://www.suicidepreventionlifeline.org/
24-hour, toll-free, confidential suicide prevention hotline available to anyone in suicidal crisis or emotional distress. Your call is routed to the nearest crisis center in the national network of more than 150 crisis centers.
SAMHSA (Substance Abuse and Mental Health Services Administration) – US: 1-800-662-HELP (4357)
http://www.samhsa.gov/find-help
SAMHSA offers 24-hour free and confidential treatment referral and information about mental and/or substance use disorders, prevention, and recovery. They also have a Disaster Distress helpline and a Veteran’s Crisis Line.

Psychedelic Safety Institute